Reopening pulmonary function services during COVID-19

In the spring of 2020, the SARS-CoV-2 pandemic was just beginning to take hold in the United States and disrupt virtually every aspect of care delivery. We had very little understanding of how this novel virus was transmitted, how far it could spread, or even how to keep our patients safe in situations we used to take for granted. Because of this, a variety of expert groups recommended suspending “non-essential” clinical tasks including most screening and diagnostic testing procedures (including pulmonary function testing). Half a year later, many questions regarding SARS-CoV-2 remain unanswered, but we do now have a clearer picture of how to minimize the risk to our patients. To that end, the American Thoracic Society has published the advice of an expert working group to guide PFT labs and practices performing office spirometry get back to the essential work of properly diagnosing and managing our patients with dyspnea.
Flexibility is key #
First and foremost, practices must remain flexible and ready to adapt to changing circumstances. The pandemic itself is made up of clusters of smaller outbreaks that are affected by an enormous number of regional variables, including demographics, local health policy, and social factors. Practices must remain agile enough to adapt to changing circumstances, as well as understand that what works in one system or region might not be the best solution for another.
When to resume testing #
So how does a practice know conditions may be right for a safe reopening? Guidance from the Centers for Medicare and Medicaid Services (CMS) states that the same ‘gating’ criteria the Centers for Disease Control and Prevention (CDC) use for reopening in general are appropriate here; that is, a downward trajectory of COVID-19 cases (as well as COVID-19-like illnesses) over a 14-day period. This also means that local testing infrastructure has to remain solid and consistent, and it’s a wise idea to use rolling averages for cases (rather than daily case reports) in order to even out variations in testing volumes. In places where COVID-19 numbers are relatively low to begin with (thus making it more difficult to trend downward), flat trends may be used instead. As long as cases aren’t increasing, and healthcare systems aren’t facing imminent crises, practices should consider resuming testing.
Reducing the risk on-site #
Our knowledge regarding SARS-CoV-2 is evolving, and many controversies remain regarding how the virus is spread and exactly what the risk is for various PFT procedures; therefore, it is most appropriate to assume every patient is a potential carrier in order to reduce the risk of clinicians (or other patients) being exposed.
The first step is a consistent screening procedure looking at any potential exposures or symptoms. The ATS working group’s paper suggests this screening should occur within 72 hours of the schedule test in order to minimize post-screening exposure and “false negatives” brought on by late development of symptoms. Patients who trigger screening questions should then be referred for SARS-CoV-2 testing within 48 hours of their appointment. This is yet another area where local conditions will impact scheduling, as availability of testing is still inconsistent across the country, and many of our people living with chronic respiratory conditions have symptoms consistent with COVID-19 at baseline. Adding PFT subjects to the mix has the potential to strain local testing infrastructure, but is again critical out of an abundance of caution.
Assuming the patient clears testing, that abundant caution should still continue all the way through the day of testing. Upon entrance to the facility, patients should be screened once again for symptoms that may have developed since the initial questionnaire. The working group’s recommendations state that temperature checks are appropriate if resources allow, but the accuracy of some non-contact thermometers has been called into question, and there are a wide variety of factors that can confound readings, so patients should still be asked directly again about new-onset symptoms. If they clear this second round of screening, they can proceed to an area of the waiting room designated for low-risk patients.
The situation is a little trickier if a patient fails the screening or testing at any point. Obviously, if a patient tests positive before arriving on-site, the PFT should be rescheduled until after the infection resolves (usually indicated by either a reduction in symptoms for 72 hours with a total of 10 days after onset or two consecutive negative tests). If a patient arrives for their test with new-onset symptoms, they should be immediately removed from the usual patient flow and isolated for further evaluation. While a rapid antigen test that provides results in as little as 15 minutes has received an Emergency Use Authorization from the US Food & Drug Administration, these tests may not be available in all areas and like all tests carry the risk of false negative results. This means clinicians must again carefully weigh the benefit of testing against the risks of allowing a symptomatic patient to proceed into the facility. Again, factors like the availability of PPE and the clinical urgency of diagnosis will weigh heavily on this decision.
Infection control precautions #
As mentioned earlier, reduced operational capacity is inevitable for many practices even under the conditions that allow resumption of testing services, due to the requirements of physical distancing. Facilities will likely need to consider reducing the overall number of people in the building at any one time, and the easiest way to accomplish that is by restricting patient companions and asking them to remain outside. Patients themselves may be asked to wait outside as well; some practices are taking inspiration from the restaurant industry and using text messaging to inform patients when their appointment is ready to start.
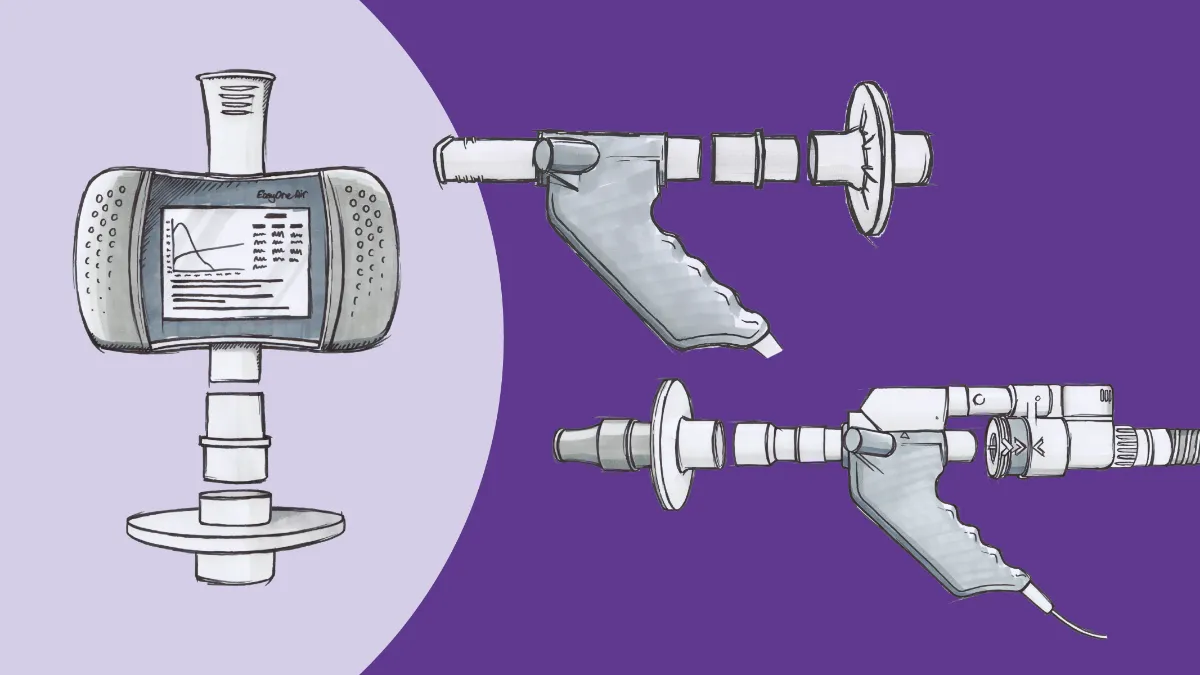
Reducing the number of appointments per day is another consideration. Greater benefit is likely seen through allowing more complete air exchange in the testing rooms. Debate rages on about the role of aerosols in the transmission of this virus, but again good practice calls for minimizing uncertain risks. Along the same lines, moving PFT equipment into negative-pressure rooms, installing ultraviolet light sanitizers, and similar strategies for viral eradication have been suggested (albeit with limited research to support their widespread use), and the use of MDIs rather than nebulized bronchodilators during pre/post bronchodilator testing has been suggested to reduce aerosol exposure.
Of course, even with fewer patients, the testing team still needs appropriate PPE in the testing room and throughout the rest of the facility. For example, cardiopulmonary exercise testing (CPET) may carry a higher risk due to the time it takes to complete the test and more forceful breathing, where basic spirometry is less risky (but by no means risk-free due to proximity and provocation of cough). The ATS working group suggests a mask for pre-testing interviews and discussion, then adding a gown, gloves, and face shield for the actual testing procedures. Patients, of course, should be masked at all times other than when they are performing maneuvers.
The road ahead #
The pandemic has impacted every aspect of healthcare delivery, and pulmonary function testing is no exception. The initial concerns regarding patient safety that led to widespread disruption in services early in the pandemic have obviously not gone away, but they are increasingly accompanied by concerns about the disservice done to patients by indefinitely delaying accurate diagnosis. It’s now time to recognize that there are ways to provide these critical services in ways that minimize risk and inform better clinical decision-making. In addition, the next few years will likely see major technological innovations that not only reduce the risk further, but bring the promise of high-quality pulmonary testing to more people, allowing for improvements in detection and management for a variety of chronic conditions, as well as discovering any long-term lung function impairments that develop as a result of COVID-19. Despite the confusion and uncertainty that currently reigns in the PFT world, the post-pandemic future looks incredibly bright!