The role of lung transplantation in the battle against COVID-19

It often seems like there ‘aren’t many lights’ in the darkness of the COVID-19 pandemic.
As of this writing, cases are once again surging around the world. We look ahead to a radically different holiday season, and there is still much uncertainty about things ever returning to ’normal’ but there are positive stories, as well.
● We are learning more about how the virus impacts physiology.
● More effective treatments are being discovered.
● As a result, the mortality rate appears to be dropping.
In that spirit, it’s time to look at one of the most heroic efforts being done to save lives: lung transplantation in COVID-19 patients.
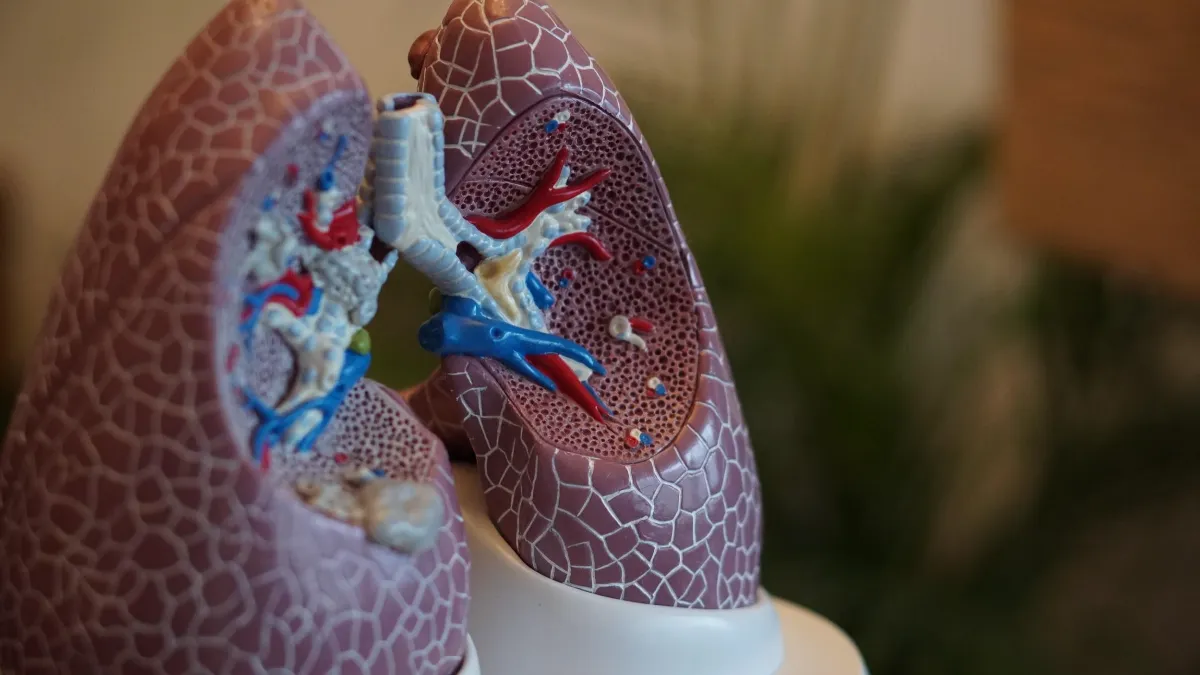
When are lung transplants a viable option? #
Historically, lung transplants have been used to prolong the lives of people nearing the end of advancedchronic lung conditions such as emphysema, bronchiectasis, or cystic fibrosis1. Indeed, the current eligibility criteria for many transplant centers still specifically highlights these conditions.
The idea is that the risk of such an invasive, fundamentally transformative procedure is simply too high unless there is absolutely no chance the lungs will recover on their own. This risk also presents challenges for selecting the best possible candidates for the limited selection of donor organs available. Thus, the list of potential contraindications is far longer than the inclusion criteria.
What are the criteria for lung transplant eligibility? #
Optimal candidates must be tobacco-free for at least six months, they must be in a healthy weight range, they must have psychosocial support, and so on. All these things take time to evaluate and consider before someone is placed on the transplant list.
In the case of Johns Hopkins Medicine, their Comprehensive Transplant Center also lists “severe local or systemic infection” as one of the necessary lung transplant contraindications. That seems somewhat obvious, considering the very act of transplanting an organ exposes someone to a significant risk of additional infection and requires ongoing immunosuppression. However, it also seems to exclude patients enduring COVID-19 from consideration.
After all, how could it possibly be safe to suppress the immune system of someone already dealing with a raging infection? And how can transplant teams properly assess all the other relative contraindications to maximize the chances of a positive outcome?
Is lung transplantation a viable solution in COVID-19? #
Desperate times call for desperate measures, and as Captain Jean-Luc Picard of Star Trek: The Next Generation once said, “Things are only impossible until they are not.” That has led surgeons like Northwestern Memorial Hospital’s Chief of Thoracic Surgery, Dr. Ankit Bharat, to reconsider the use of transplantation for the most severe cases of COVID-19.
Two of Dr. Bharat’s patients, the very first recipients of COVID-19-related double-lung transplants, were interviewed earlier this year for several news outlets, including the New York Times2. Theirs are stories of perseverance and hope during the pandemic.
The two came to Northwestern Memorial with vastly different backstories. Mayra Ramirez was a 28-year-old working as a paralegal for a Chicago law firm. She was on a medication that potentially muted her immune response, so when the first shelter-in-place orders came through during the initial wave of the pandemic, she followed them diligently.
Brian Kuhns was a 62-year-old mechanic from Lake Zurich, Illinois, a suburb about 45 minutes from the Windy City. He admits he thought the risks of the novel coronavirus were overblown before tragically being proven wrong. He fell ill one day coming back from lunch to his auto shop, saying he felt fine until he didn’t. “Boom,” he tells it. “I was done.”
Mayra was the first to fall ill. Like many in the early days of the pandemic, she wasn’t certain her symptoms were really COVID-19. The last thing she wanted was to be admitted during a time when there were still so many unknowns and ventilation strategies were still potentially a death sentence, so she waited until the last possible minute to go into the hospital.
As she tells it, she thought she’d be there a week at most. But a week turned into a month and a half, much of it spent on a ventilator and then on extracorporeal membrane oxygenation (ECMO) as her clinicians struggled against the virus on behalf of her suppressed immune system.
Secondary infections set in, complicating the fibrosis now believed to be a component of severe COVID-19 cases. These infections caused cavitation in her lungs, and combined with the newly-stiff lung tissue surrounding the cavities, Mayra’s condition became dire.
Her family was called in from North Carolina to say goodbye.
That’s when Dr. Bharat stepped in. As the surgical director of Northwestern Medical’s lung transplant program, he knew the significant risks involved in getting Mayra new lungs. But he also knew that was her only realistic chance at survival, and at that point, there had been one reported transplant of COVID-19 lungs in Austria3. Mayra had been generally healthy prior to admission, which was in her favor, but she was also starting to show signs of multisystem organ failure.
Her family consented to Dr. Bharat’s plan, and as luck would have it, within 48 hours a pair of donor lungs became available.
Brian’s case followed a very similar path. After his wife brought him to their local hospital, the team there realized he was deteriorating rapidly and transferred him to Northwestern Memorial. There, Brian also ended up on a ventilator and an ECMO machine; in his case, for 100 days. Those days led into July 2020, just about a month after Mayra got her new lease on life. Dr. Bharat, counting the first transplant as a success at that point, offered the procedure to Brian and his family.
Once again, fortune shined upon the team and Brian was able to receive his new lungs and come off the ventilator soon after receiving the transplant4.
Can lung transplantation be used to help those with COVID-19? #
These early successes have offered some new hope to some of the most extreme COVID-19 cases. However, it has taken decades to develop best practices for transplantation evaluation in those settings where it has been done more frequently, and there is still much to learn in COVID-19 cases.
Dr. Bharat advocates for earlier recognition of severe cases, reporting one potential referral that ended up having severe pulmonary hemorrhage and kidney failure just prior to transfer, preventing them from even attempting the transplant. But determining proper timing can be tricky, as new therapeutic measures are allowing more people to recover prior to reaching the point of no return. In addition, many people with the most severe cases also tend to be those with concurrent conditions5 that make them suboptimal candidates for transplantation.
Are there any adverse effects with lung transplantation in COVID-19 patients? #
There may simply not be time to evaluate many of the psychosocial and economic considerations that are generally considered essential to good outcomes, either. After all, health concerns ‘don’t simply stop after the new organs are placed.’ Longtime COPD advocate and double-lung transplant recipient Jim Nelson has described the process as “trading one chronic condition for another,” considering the regimen of medications and precautions that are essential components of the post-transplant lifestyle.
The relatively young, relatively healthy Mayra went through months of physical and occupational therapy after her discharge, as well as home nursing care and psychological support to help cope with post-intensive care syndrome6. These services can be a tremendous strain on patients and their families, and one that many are simply not prepared to handle.
How can routine respiratory testing help with ongoing COVID-19 care? #
Ongoing testing is critical to long-term survival, as well. Lung transplants have relatively high rates of complication compared with other organs, owing to their complexity and frequent exposure to pathogens. That makes pulmonary function testing absolutely essential, as it can serve as an early-warning sign for post-transplant complications such as chronic lung allograft dysfunction (CLAD)7.
It is therefore essential that COVID-19 transplantees are able to work with a high-quality PFT laboratory capable of monitoring lung volumes and diffusion capacity for their ongoing care. This is, of course, true for any lung transplant recipient but may be particularly true considering the uncharted territory of how COVID-19 will affect other organs (like the heart) long-term and how those late effects may, in turn, affect the lungs. It will likely be many years before science can determine whether these survivors are at higher than normal risk for complications or have other unique health concerns created by their novel condition.
Pulmonary professionals will clearly be at the forefront of caring for this population for a long time to come.
Who is eligible for a COVID-19 lung transplant? #
An analysis of the limited case data available recently published in the Lancet (When to consider a lung transplant in COVID-19) offers some potential guidance to help clinicians, patients, and families in this uncharted territory8. The paper offers ten criteria to consider when deciding to consider a COVID-19 related transplant, integrating the body of knowledge regarding transplants in general with international COVID-19-specific experiences.
Candidates should be 65 years of age or younger, as was the case with Mayra and Brian, and have only single-organ failure. Transplant should be considered no less than 4-6 weeks after the initial diagnosis of respiratory failure, allowing a reasonable timeframe for medical recovery before surgical intervention. The candidate should also be essentially free of severe comorbidities (such as coronary artery disease), be free of the SARS-CoV-2 virus itself (as determined by PCR testing), and be able to participate with some degree of physical rehabilitation during their time on the waiting list.
The transplant center doing the procedure should have extensive experience with high-risk transplants and have a relatively low waiting-list mortality rate, demonstrating high-quality pre-operative care. Finally, in recognition of the aforementioned psychological demands of the post-transplant lifestyle, the paper strongly recommends that not only the family be involved, but the patient themselves be part of the decision-making process. The authors point out that the stress of going to sleep with respiratory failure, being under for weeks at a time (like Mayra and Brian), and waking up with a new set of organs and lifetime of immunosuppression can be, as they put it, “psychologically traumatic and sometimes insurmountable.”
Will lung transplantation change how we can care for COVID-19 patients? #
Despite all the challenges and unknowns, surgeons like Dr. Ankit Bharat have given a glimmer of hope where there was once only a sense of futility. Following his example, transplant centers around the world have also begun transplanting lungs into their most critical cases. Data is limited as to the number of people who have received new lungs, but centers in Florida, Texas, and Tennessee are reporting they have either completed at least one transplant or are on the cusp of an attempted COVID-19 lung transplant.9
It seems likely that as the pandemic becomes resurgent through winter in the Northern Hemisphere, more patients will become potential candidates, more families will consider taking on the risks and burdens, and more facilities will be called upon to perform the procedure and provide the necessary follow-up care. Each procedure will add to our body of knowledge, as well as add to the number of people allowed to turn mere hope into long-term survival.
Lung Transplant Patient Selection Criteria - Johns Hopkins Comprehensive Transplant Center. (Accessed November 2, 2020) ↩︎
A COVID-19 Patient Goes Home After a Rare Double Lung Transplant - The New York Times (Accessed November 2, 2020). ↩︎
Europe’s First Lung Transplant on a Coronavirus Patient - Cath Lab Digest (Accessed November 2, 2020). ↩︎
Grandfather who survived COVID-19 recalls life-saving double lung transplant: “I took a chance” - CBS News (Accessed November 2, 2020). ↩︎
Scientific Evidence for Conditions that Increase Risk of Severe Illness - COVID-19 - CDC (Accessed November 2, 2020). ↩︎
COVID-19 Patient Who Received Double-Lung Transplant Faces Long Road To Recovery - Illinois Newsroom (Accessed November 2, 2020). ↩︎
Singer LG. Physiologic changes following lung transplantation Physiologic changes following lung transplantation. 2015:1-16 - Up To Date (Accessed November 2, 2020). ↩︎
Cypel M, Keshavjee S. When to consider lung transplantation for COVID-19. Lancet Respir Med. 2020;8(10):944-946. doi:10.1016/S2213-2600(20)30393-3 ↩︎
‘We’re poised to do it’: University Hospital to perform double lung transplants for COVID-19 patients with irreversible lung damage - ExpressNews.com (Accessed November 2, 2020). ↩︎