Confidence in uncertain times

It’s been a long year and a half.
The COVID-19 pandemic has wreaked havoc with many aspects of our lives that we previously took for granted. We’ve changed not only the way we work, but the way we play, the way we consume media, often even the way we shop. Despite our efforts, we continue to see tremendous uncertainty regarding the next phases of this public health emergency. Many parts of the country are seeing new surges in caseloads, once again straining local healthcare systems to the brink. We’re seeing the effects of long COVID continuing to loom, affecting the lives of those who were hopeful to escape with only a ‘mild’ case. New variants, with uncertain levels of communicability, severity, and potential resistance to vaccines are continually on the radar.
However, we also have to consider that COVID-19 isn’t the only game in town. While it’s certainly the condition that gets the most news, things like asthma and COPD haven’t gone away. These populations continue to need the high-quality, individualized care they’ve always called upon pulmonary professionals for, starting with accurate diagnostics. Pulmonary function testingcontinues to stand at the heart of individualized treatment plans for asthma, COPD, cystic fibrosis, and a score of other respiratory disorders. In addition, COVID long-haulers need access to testing to evaluate trends in their condition, as well as provide valuable research data.
Pulmonary function testing (PFT) you can count on #
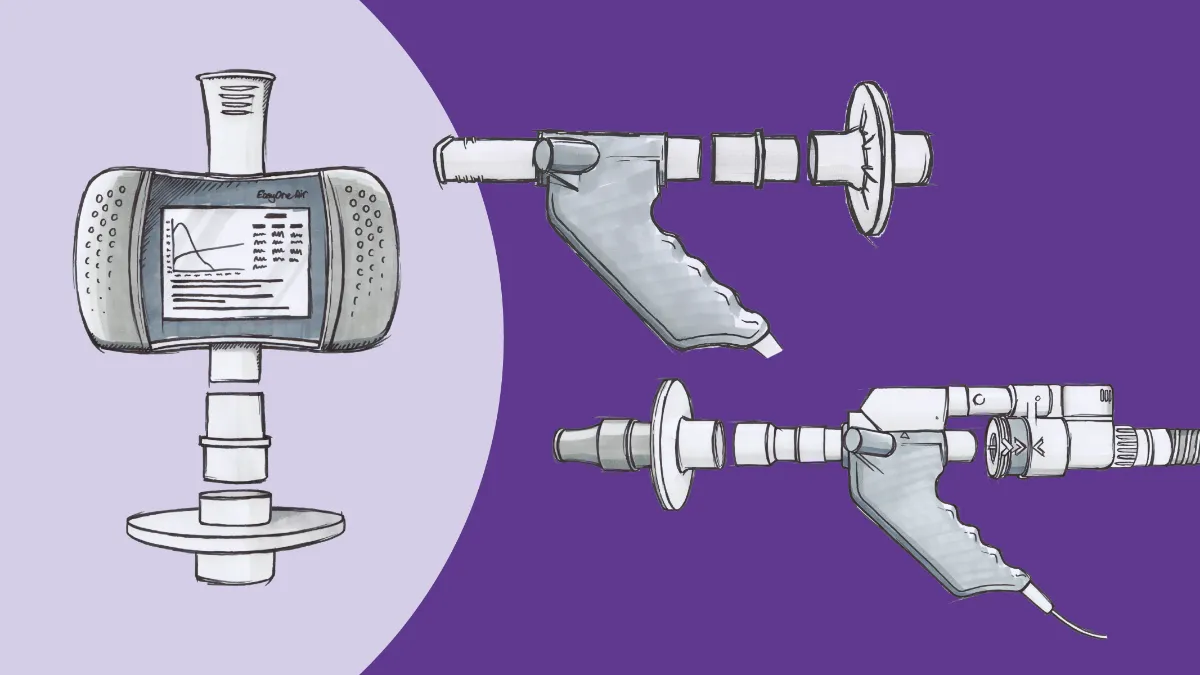
Fortunately, pulmonary function testing is one thing you can still absolutely rely upon. During the last year, we’ve extensively covered the many ways pulmonary function programs can continue to see patients safely, from how to reopen your workflows to best practices for PFTs during the pandemic to expanding PFT services outside the traditional laboratory setting. ndd also produced a roundtable webinar with tips and tricks for re-establishing routine PFT services. Fortunately, what we know about how to perform PFTs during the pandemic has remained surprisingly stable, especially given the ever-evolving evidence we’ve seen in, for example, COVID-19 treatment. With proper safety and cleaning procedures in place, it is entirely feasible to have fully functioning PFT programs. As providing maximum safety remains a top priority during the pandemic, additional infection control options, such as ndd’s single-use inline filter solutions, have been developed and implemented. These allow another layer of protection and confidence that your patients and staff will remain as safe as possible, while still allowing your practice to provide an outstanding level of respiratory care.
Expanding pulmonary function testing #
Of course, it’s not enough to simply maintain the status quo. As a recent white paper indicated, there appears to be a link between COVID-19 and a patient’s diffusion capacity of the lung for carbon monoxide (DLCO) measurements. It’s unclear exactly what causes these changes, although it appears to be a combination of fibrosis-like changes in the lung itself, combined with issues with the pulmonary vasculature and circulation. These kinds of changes can contribute to lower blood oxygenation, which in turn can lead to tissue hypoxia and inflammation throughout the body. Persistent hypoxia and inflammation have previously been associated with symptoms like those reported in long COVID, including chronic fatigue and neurological deficits (sometimes called ‘brain fog’).
Considering that over a third of those enduring long COVID had mild enough cases that they didn’t need to be hospitalized, there may be an entire cohort of people who have the effects of long COVID but haven’t put together that their exposure to the virus is what’s making them feel bad. This is an opportunity for primary care practices and ambulatory clinics to shine. By implementing point-of-care pulmonary function testing (particularly DLCO testing) programs, such practices can more easily identify COVID long-haulers and begin developing appropriate treatment plans to get them back to full function. Such point of care testing is more important than ever, and more feasible with low maintenance, high precision technology, advancing to the point of portability (for example, the ndd EasyOne Pro). With these PFT testing solutions, pulmonary function testing measurements can become as much as part of routine biometric assessments as blood pressure and weight checks.
This expanded testing can have significant positive impacts outside of COVID-19 as well. For example, epidemiological data suggest that as many as 13 million people in the US may be walking around with COPD but have never been diagnosed.1 As the airflow limitation inherent in COPD steadily worsens, people adjust their habits and lifestyle to accommodate their decreased endurance. This leads to many people not getting proper care until relatively advanced stages of the condition. However, routine spirometry and pulmonary function testing in the clinic setting could lead to much earlier detection, and thus earlier intervention to slow disease progression. Similarly, spirometry and other PFTs can aid in the diagnosis of a variety of other cardiopulmonary conditions, from asthma to cardiac issues.
Certainty in uncertain times #
The road ahead certainly seems fraught with challenges. The Delta variant of COVID-19 has unfortunately flashed us back to the earlier days of the pandemic, and we don’t know if another variant could do the same once we get Delta better controlled. Public health is facing enormous challenges with communication and dissemination of best practices, especially in the face of persistent misinformation. Healthcare providers are overwhelmed and frustrated, and it may seem like, as the song goes, there’s too much confusion and we can’t get no relief. However, one thing actually IS absolutely certain: The role of pulmonary function testing is not only here to stay, but poised to expand dramatically. Cutting-edge practices are already beginning to implement point-of-care testing into their workflows, improving patient care and outcomes. The time to join them, and make an impact on COVID-19 and beyond, is right now.
Haroon S, Adab P, Riley RD, Fitzmaurice D, Jordan RE. Predicting risk of undiagnosed COPD: development and validation of the TargetCOPD score. Eur Respir J. 2017;49(6):1602191. doi:10.1183/13993003.02191-2016 ↩︎