DLCO as a cornerstone for long-COVID management
The COVID-19 pandemic has gripped the entire globe and has impaired millions of victims worldwide. The virus affects the respiratory system of patients culminating in inflammation, lung damage and pneumonia in many cases. Time is a crucial parameter as the pandemic unfolds and its aftermath on the patients is what clinicians are most concerned about. There are clear indications that many patients recuperating from COVID-19 infection continue to have persistent symptoms and lower lung function complications long after their recovery.
Similar pandemics in the past such as the SARS and the MERS have shown that patients who recovered from those diseases continue to have long-term complaints and lung damage even several years post recovery.1 The pathogen that caused SARS and MERS closely resembles that of COVID-19 albeit with lesser virulence and contagion. Hence it is expected that the patients recovering from the current pandemic will have similar/more ailments in the long run.
Hence monitoring of pulmonary function in patients recovering from COVID-19 (both severe and mild) is extremely essential for long-term patient management. Till now most of the research has been able to point towards the post-COVID pulmonary sequelae within the first 3 months after recovery to a limited number of patients and time. In this blog, we only focus on relatively longer periods of post-COVID recovery and follow-up to obtain better insights into the pathophysiology of the disease and its remission.
Consistent structural and functional lung damage in COVID patients 12 months from recovery #
To evaluate the long-term effects of COVID 19, Xiaojun Wu et al. conducted a prospective, longitudinal, follow-up study whereby COVID hospitalized patients were followed up until 12 months after recovery.2
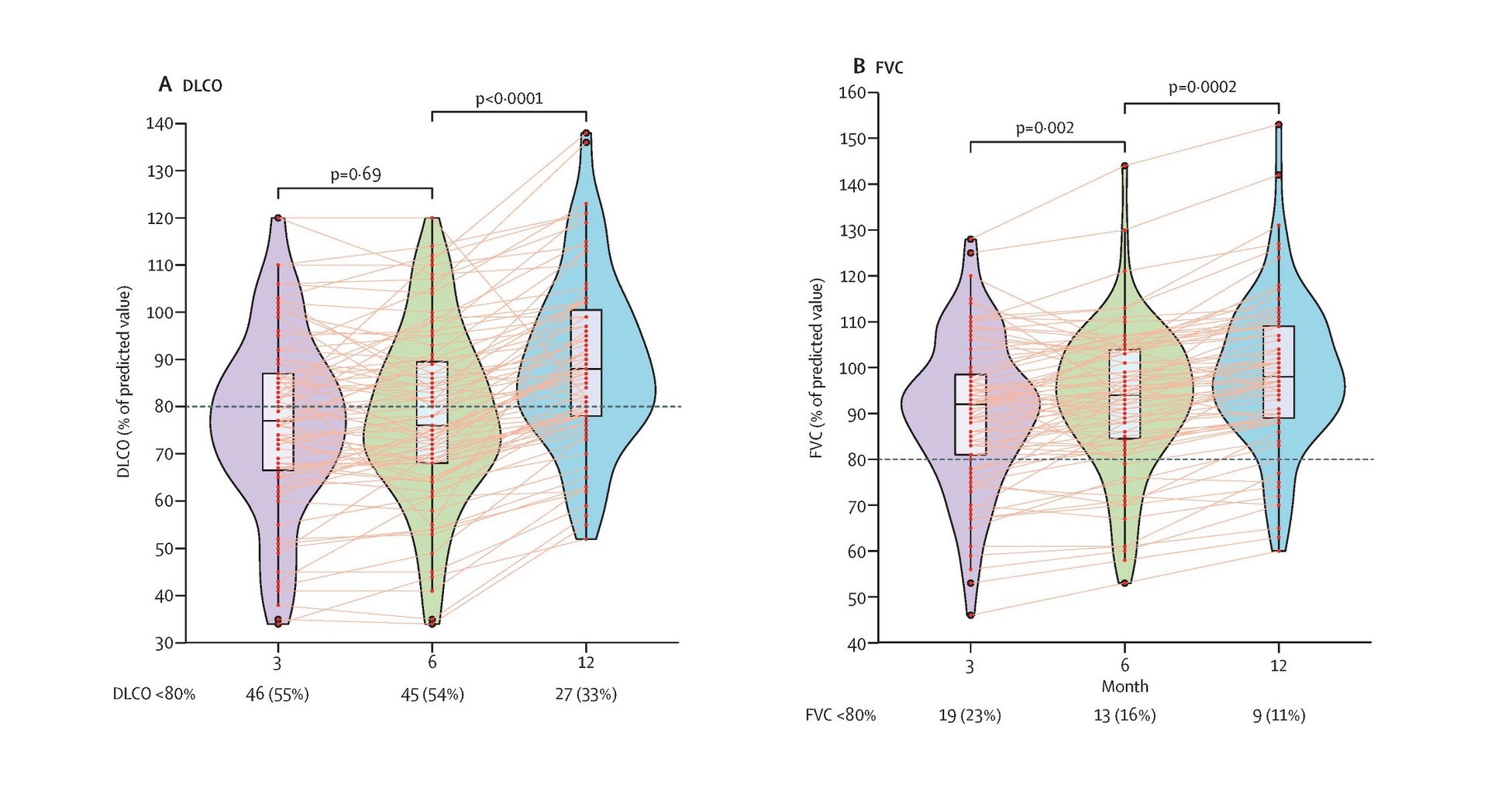
Figure pictured above: Violin plots showing temporal changes in lung function in patients recovering from severe COVID -19 related hospitalization. Data represented here are median (IQR). The figure shows n (%) of patients with abnormal DLCO or FVC. Horizontal dotted lines indicate the normal cut-off at 80%. DLCO=diffusing capacity of the lungs for carbon monoxide. FVC=forced vital capacity.
Pulmonary function tests including DLCO and FVC measurements were performed in all patients at 3 months, 6 months, and 12 months following COVID-19 related hospital discharge. Patients showed improvement reflected in DLCO and FVC (% predicted) from 3 months up to 12 months after discharge from the hospital. A sub-group of severe patients had persistent abnormalities in lung function even after 12 months (Data not shown in this figure). This indicates the importance of long-term follow-up of COVID patients post-recovery using the information from lung function indices especially DLCO.
Study design: Pulmonary function, exercise capacity, and chest High-Resolution Computed Tomography (HRCT) were recorded in 83 non-intubated patients hospitalized with severe COVID-19 pneumonia at 3, 6, 9, and 12 months following their discharge.
Results: Persistent physiological and radiographic abnormalities remained for a long in some patients with COVID-19 even after 12 months from discharge.
Pulmonary abnormalities resulting in a reduction in gas transfer of lungs as measured by the diffusing capacity for carbon monoxide (DLCO) were significant in certain patients. This effect could be confirmed by published literature stating that blood gas exchange has been observed to be impaired in patients who have been discharged following hospital admission with COVID-19 pneumonia.3
Findings: This study was consistent with a previous COVID-19 follow-up study at 6 months. It also validated a recent report to identify that female sex strongly predicts impaired DLCO at 6 months after recovery and extended the findings up to 12 months post discharge.4 Although DLCO was associated with the female sex, HRCT was not, suggesting that distinct mechanisms could culminate in lung function (DLCO) and structural (HRCT) damage. At 12 months after discharge, fibrosis along with the presence of interstitial thickening and reticular opacity was observed, indicating the persistence of radiological damage in one-fourth of the patients.
Take home message/s: The findings highlight the importance of respiratory follow-up of patients with COVID-19 especially routine DLCO tests which are accessible and relatively cheap to assess lung improvement aiding better patient management and diagnosis of collateral lung damage.
Physiological and psychological stress post COVID infection: DLCO emerges as a potent indicator of physiological damage #
Studies with lesser follow-up time such as the one published by Mattia Bellan et al. in JAMA Network open also point towards the importance of lung function (indicated by DLCO) testing in long-term COVID management post-recovery.5
Objective: This particular research was conducted to evaluate the extent of lung function impairment, exercise function, and psychological impact among patients who recovered from COVID, 4 months after discharge.
Findings: A significant proportion of survivors of COVID-19 experienced respiratory or functional impairment 4 months after hospital discharge, with clinically relevant psychological consequences. Greater than 50% of the participants had DLCO less than 80% of expected at the end of follow-up, indicating a significantly impaired diffusion amongst the survivors of COVID-19. DLCO reduction happens to be the most common functional alteration reported in patients with COVID-19. This can be reflected in the isolated reduction of DLCO with the preservation of other PFT parameters. A reduction of DLCO has been previously associated with pulmonary fibrosis in different clinical settings, such as interstitial lung diseases and systemic sclerosis.6 Whether COVID-19 related reduction of DLCO also leads to pulmonary fibrosis thereafter needs to be further investigated although fibrotic indications have been linked to SARS before.7
Take home message/s: Not only physical and physiological but also psychological sequelae prevailed 4 months after discharge among patients who had been hospitalized for COVID-19. DLCO was the most important parameter that revealed physiological damage to the lungs in these patients advocating the utility of the measurement in COVID management.
DLCO reveals significant lung impairment in COVID patients with severe dyspnea #
A study performed by Cortes-Telles et al. examined the physiological mechanisms of persistent respiratory distress (dyspnea) in COVID-19 survivors.8 Survivors from the pandemic seem to have varying degrees of dyspnea. The authors included 186 non-critical COVID-19 patients with varying degrees of persistent symptoms between 30 and 90 days following the onset of symptoms. Patients were divided into those with (n = 70) and without (n = 116) persistent dyspnea. Significantly lower DLCO, reduced functional capacity, oxygen saturation, and fatigue emerged as the characteristics of patients with-dyspnea as opposed to without-dyspnea phenotypes. This suggests that there is a true physiological mechanism that may explain persistent dyspnea after COVID-19 and regular follow-up of patient lung function could prove potential in better management.
Take home message/s: Significant lung damage indicated by the diffusing capacity for carbon monoxide, long after recovery was apparent in those group of COVID patients who had severe symptoms. Hence these group of patients are expected to benefit the most from regular follow-up of their DLCO after COVID infection.
DLCO: Long way to go in COVID #
Finally, another study published by Zhang and colleagues describes the long-term health outcomes of patients with COVID-19 and investigates the potential risk factors.9
40 patients (including 25 severe cases) were enrolled in the study and thereafter followed up approximately after 8 months from hospital discharge.
Findings: At follow-up, severe cases had higher incidences of persistent symptoms, DLCO impairment, and higher abnormal CT scores as compared with mild cases. A CT or computed tomography scan is a sophisticated imaging technique used especially in the field of radiology and beyond to obtain high resolution non-invasive images of for our body for diagnostics.
Percent predicted DLCO at follow-up was negatively correlated with cumulative days of oxygen treatment during hospitalization. The ratio of DLCO to alveolar ventilation (percent predicted DLCO/VA) at follow-up was positively correlated with patients’ BMI and a pro-inflammatory cytokine marker Tumour Necrosis Factor-alpha (TNF-α). TNF- α has already been proven to be a strong indicator of patient survival in the context of COVID and implicated in treatment regimen.10
Take home message/s: This study again demonstrates that survivors with severe COVID-19 had higher incidences of DLCO impairment, persistent daily symptoms, and higher abnormal CT scores as compared with mild cases. It also leads to a hypothesis that either absence or excess of inflammation during the COVID-19 course would probably lead to the impairment of pulmonary diffusion function.
Conclusion: Keeping in mind the findings of the above-mentioned studies pulmonary function (especially diffusion capacity as measured by DLCO) seems to be the most crucial of the parameters that continue to lag with patient’s recovery. Hence, management strategies post COVID should embrace regular monitoring of pulmonary function (especially DLCO testing) as the cornerstone of patient management for the recovered.
Other long-term effects such as fibrosis etc. need to be evaluated with more time post-recovery.
Ahmed, H.; Patel, K.; Greenwood, D. C.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; Sivan, M., Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J Rehabil Med 2020, 52, (5), jrm00063. ↩︎
Wu, X.; Liu, X.; Zhou, Y.; Yu, H.; Li, R.; Zhan, Q.; Ni, F.; Fang, S.; Lu, Y.; Ding, X.; Liu, H.; Ewing, R. M.; Jones, M. G.; Hu, Y.; Nie, H.; Wang, Y., 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalisation: a prospective study. Lancet Respir Med 2021, 9, (7), 747-754. ↩︎
- Qin, W.; Chen, S.; Zhang, Y.; Dong, F.; Zhang, Z.; Hu, B.; Zhu, Z.; Li, F.; Wang, X.; Wang, Y.; Zhen, K.; Wang, J.; Wan, Y.; Li, H.; Elalamy, I.; Li, C.; Zhai, Z.; Wang, C., Diffusion capacity abnormalities for carbon monoxide in patients with COVID-19 at 3-month follow-up. The European respiratory journal 2021, 58, (1).
- Shah, A. S.; Wong, A. W.; Hague, C. J.; Murphy, D. T.; Johnston, J. C.; Ryerson, C. J.; Carlsten, C., A prospective study of 12-week respiratory outcomes in COVID-19-related hospitalisations. Thorax 2021, 76, (4), 402-404.
- Zhao, Y. M.; Shang, Y. M.; Song, W. B.; Li, Q. Q.; Xie, H.; Xu, Q. F.; Jia, J. L.; Li, L. M.; Mao, H. L.; Zhou, X. M.; Luo, H.; Gao, Y. F.; Xu, A. G., Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine 2020, 25, 100463.
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; Luo, J.; Huang, Z.; Tu, S.; Zhao, Y.; Chen, L.; Xu, D.; Li, Y.; Li, C.; Peng, L.; Li, Y.; Xie, W.; Cui, D.; Shang, L.; Fan, G.; Xu, J.; Wang, G.; Wang, Y.; Zhong, J.; Wang, C.; Wang, J.; Zhang, D.; Cao, B., 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021, 397, (10270), 220-232.
Bellan, M.; Soddu, D.; Balbo, P. E.; Baricich, A.; Zeppegno, P.; Avanzi, G. C.; Baldon, G.; Bartolomei, G.; Battaglia, M.; Battistini, S.; Binda, V.; Borg, M.; Cantaluppi, V.; Castello, L. M.; Clivati, E.; Cisari, C.; Costanzo, M.; Croce, A.; Cuneo, D.; De Benedittis, C.; De Vecchi, S.; Feggi, A.; Gai, M.; Gambaro, E.; Gattoni, E.; Gramaglia, C.; Grisafi, L.; Guerriero, C.; Hayden, E.; Jona, A.; Invernizzi, M.; Lorenzini, L.; Loreti, L.; Martelli, M.; Marzullo, P.; Matino, E.; Panero, A.; Parachini, E.; Patrucco, F.; Patti, G.; Pirovano, A.; Prosperini, P.; Quaglino, R.; Rigamonti, C.; Sainaghi, P. P.; Vecchi, C.; Zecca, E.; Pirisi, M., Respiratory and Psychophysical Sequelae Among Patients With COVID-19 Four Months After Hospital Discharge. JAMA Netw Open 2021, 4, (1), e2036142. ↩︎
Nihtyanova, S. I.; Schreiber, B. E.; Ong, V. H.; Rosenberg, D.; Moinzadeh, P.; Coghlan, J. G.; Wells, A. U.; Denton, C. P., Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheumatol 2014, 66, (6), 1625-35.
Martinez, F. J.; Flaherty, K., Pulmonary function testing in idiopathic interstitial pneumonias. Proc Am Thorac Soc 2006, 3, (4), 315-21. ↩︎Xie, L.; Liu, Y.; Fan, B.; Xiao, Y.; Tian, Q.; Chen, L.; Zhao, H.; Chen, W., Dynamic changes of serum SARS-coronavirus IgG, pulmonary function and radiography in patients recovering from SARS after hospital discharge. Respir Res 2005, 6, 5. ↩︎
Cortes-Telles, A.; Lopez-Romero, S.; Figueroa-Hurtado, E.; Pou-Aguilar, Y. N.; Wong, A. W.; Milne, K. M.; Ryerson, C. J.; Guenette, J. A., Pulmonary function and functional capacity in COVID-19 survivors with persistent dyspnoea. Respir Physiol Neurobiol 2021, 288, 103644. ↩︎
Zhang, S.; Bai, W.; Yue, J.; Qin, L.; Zhang, C.; Xu, S.; Liu, X.; Ni, W.; Xie, M., Eight months follow-up study on pulmonary function, lung radiographic, and related physiological characteristics in COVID-19 survivors. Sci Rep 2021, 11, (1), 13854. ↩︎
Del Valle, D. M.; Kim-Schulze, S.; Huang, H. H.; Beckmann, N. D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T. H.; Madduri, D.; Stock, A.; Marron, T. U.; Xie, H.; Patel, M.; Tuballes, K.; Van Oekelen, O.; Rahman, A.; Kovatch, P.; Aberg, J. A.; Schadt, E.; Jagannath, S.; Mazumdar, M.; Charney, A. W.; Firpo-Betancourt, A.; Mendu, D. R.; Jhang, J.; Reich, D.; Sigel, K.; Cordon-Cardo, C.; Feldmann, M.; Parekh, S.; Merad, M.; Gnjatic, S., An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med 2020, 26, (10), 1636-1643. ↩︎