DLCO - The underutilized lung function

Despite its complexity, the functions of the pulmonary system can be essentially distilled into three main groups:
- Moving gas in and out of the lungs (or, as one of my respiratory instructors used to put it, “good air in and bad air out”).
- Holding the volume gas for a few moments to enable respiration.
- Facilitating the transfer of oxygen and carbon dioxide in and out of the bloodstream.
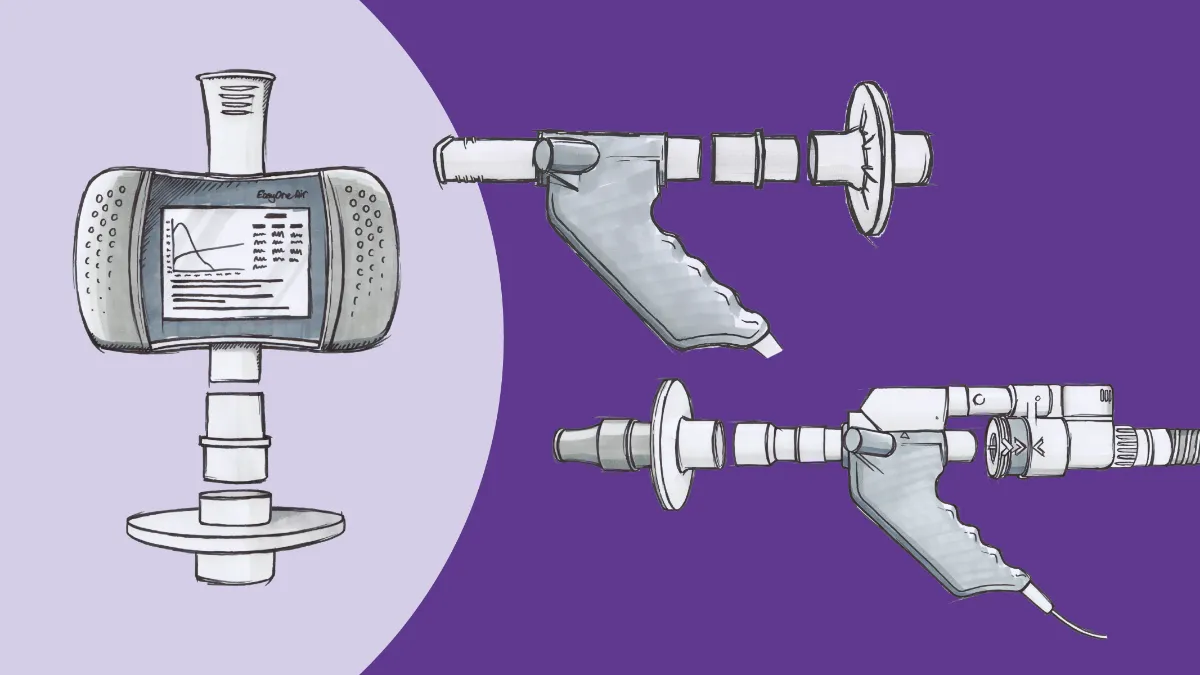
Virtually every clinician is at least familiar with the concept of measuring how well gas is physically moving in and out of the lungs, or what we call spirometry. Spirometry is still generally widely under-utilized in primary care for the diagnosis of chronic respiratory conditions, but most in practice understand what to do with the numbers when they’re available.1 Similarly, the concepts of lung volumes is long established as a thing to consider for disease management and would seem to be a valuable thing to measure and evaluate.
Except…they generally aren’t. Entire peer-reviewed papers have been written concerning the clinical significance of lung volume measurements that, while accurate and insightful in general, offer no real practical clinical implications of abnormal measurements.2 To be clear, that is no indictment of the authors of these papers; rather, they simply have virtually nothing to work with. The mechanics behind lung volumes/capacities and their interactions with respiratory dynamics can be examined and parsed, but to what end? No less an expert than Gregg Ruppel, MEd, RRT, RPFT, who wrote the book on PFTs (Ruppel’s Manual of Pulmonary Function Testing) once wrote, “Lung volumes are considered part of a complete pulmonary function test, but their value for enhancing clinical decision making is unknown. 3Even though it’s been close to a decade since those words were published, we’re not really any closer to putting them to practical use outside of research.
Land of diffusion #
That brings us to evaluating how well oxygen molecules move from the alveoli and into the bloodstream. This measurement, called diffusion (or sometimes transfer) capacity of carbon monoxide (DLCO/TLCO) actually does provide a great deal of clinical insight into several disease processes. The utility of DLCO measurements is what has led them to be performed at nearly five times the rate of lung volume testing, yet much like spirometry this measurement is still as under-utilized as it is under-appreciated.
This utility springs from DLCO’s ability to look at the entire respiratory membrane, which consists of the alveolar endothelium, the vascular endothelium, and the basement membrane they share.4 This boundary is less than a micrometer thick, allowing for oxygen and carbon dioxide to literally diffuse across it. However, that diffusion can also be affected by several other factors. In emphysema, alveolar coalescence reduces the surface area of the alveoli, providing fewer opportunities for molecules to make their respective trips. Thickening of the respiratory membrane (as in interstitial lung disease (ILD)) makes it more difficult for the molecules to move across, resulting in the hypoxemia that is a hallmark of ILDs like pulmonary fibrosis. Blood supply issues can affect the rate of transfer as well, with lack of circulation (as in chronic pulmonary emboli) reducing opportunities for gas movement, and increased blood flow (as seen with the inflammation of asthma) actually increasing that movement.
That makes DLCO invaluable across the spectrum of lung pathologies. The measurement is probably most well known in interstitial lung disease circles, where that respiratory membrane thickening is the critical issue. Here, decreases in DLCO can serve as an early-warning flag for conditions like idiopathic pulmonary fibrosis (IPF) even before spirometric changes can be seen (and therefore potentially even before symptoms manifest).5 This means DLCO should become a standard test for anyone at risk for developing these kind of interstitial conditions, such as those patients beginning amiodarone or other medications that are associated with these risks (including several anti-infectives and newer biological therapies). DLCO has also been established as a tool for tracking the progression of these conditions and predicting mortality. A five-year study of over 700 patients listed in the European EMPIRE registry of people living with IPF found that a decline of 15% or more in someone’s DLCO over the course of a year was associated with triple the risk of death by the end of year five.6 The study authors found DLCO to be a stronger predictor of mortality compared with more conventional FVC measurements, and asserted that DLCO measurements become a standard part of care for this population.
An emerging area of interest where DLCO can be of unexpected value is looking at conditions where pulmonary blood flow is affected, since it looks at the circulatory side of respiration. A study from 2019 followed 259 patients with pulmonary hypertension diagnosed via right heart catheterization and inert gas rebreathing (to evaluate cardiac output). The study found that while expected factors such as age, 6-minute walk distance, and WHO functional class were all independent predictors of mortality, statistically the most powerful indicator was DLCO.7 This reinforced previous work that found that while changes in DLCO didn’t correlate well with hemodynamic numbers, they were quite predictive of functional parameters, and low DLCO was directly associated with poorer outcomes.8
Enhanced pulmonary circulation can impact DLCO, but in the opposite direction. Once again, allowing more opportunities for molecules to move across the respiratory membrane allows for a higher transfer coefficient, and therefore a higher diffusion capacity. This is most classically seen in inflammatory processes (such as asthma), where the increased blood supply feeding the inflammation also facilitates gas transfer. In fact, in a study of people found to have higher-than-predicted DLCO values, 62% of them were found to have a diagnosis of asthma, obesity (where the role of inflammation is often under-recognized), or both.9 There are certain other circumstances where a surplus of hemoglobin ‘boxcars’ may lead to an increased DLCO, such as polycythemia or patent foramen ovale (creating a right-to-left cardiac shunt), but these are generally more ‘zebras’ than things you’ll find commonly or even specifically due to the DLCO reading. Still, these are useful considerations to keep in the back of your mind, as a pre-existing ‘high’ condition may mask the development of a ‘low’ condition, and must be evaluated in the context of the entire patient.
The DLCO/COPD connection #
Where DLCO measurements do have a great deal of as-yet-unrealized potential is the assessment and management of COPD. The role of spirometry is very well-known here, but looking at gas transfer is a surprisingly strong second place contender, especially in people where emphysemic damage is more predominant over bronchitis and inflammation. Again, alveolar coalescence can have a big impact on the area available for gas exchange. Research from the highly-respected COPDGene project has suggested that reduced DLCO is associated with a variety of COPD-related morbidities, including increased symptom burden, decreased exercise capacity, and elevated risk of exacerbations.10 Notably, these changes were seen even controlling for FEV1 impairments or degree of emphysema on CT scan. Over the longer term, a DLCO measurement less than 40% of the predicted value suggests increased mortality, enabling clinicians to be more aggressive with advanced therapies to protect their patients.
DLCO obviously has significant diagnostic utility as well. In people who smoke and have post-bronchodilator FEV1 impairment (diagnostic of COPD), low DLCO measurements can help discriminate between people with emphysema from those with chronic refractory asthma. Similarly, restrictive lung disease (proportional reductions in both FEV1 and FVC) can be separated (with a high degree of certainty) from low effort or poor technique simply by the addition of DLCO testing, and even put clinicians on the path to diagnose disorders of the pulmonary circulation. 11This can be incredibly useful in both primary care and pulmonology settings, as these cases can be readily identified without sending patients to dedicated pulmonary function laboratories (saving both time and potential COVID-19 exposures).
Even ‘pre-COPD’ can be detected with DLCO measurements. Again drawing upon the COPDGene study, researchers have drawn a connection between small airways disease (SAD), which is often considered a precursor to emphysema, and impaired diffusion.12 SAD appears to be a major contributor to overall airways resistance in the setting of emphysema, but isn’t always detectable as obstruction on spirometry. However, it is detectable on CT scans, so researchers examined the records of patients with both DLCO and CT data available and found that DLCO could be an early-warning marker not only in interstitial disease, but obstructive ones as well.
Conclusion #
The heavy burden of COPD and other chronic respiratory conditions on the healthcare system, combined with the looming addition of long-haul COVID-19, means that clinicians need every piece of information possible to provide optimal care. We can no longer afford to overlook any test or data point, including those that have historically been the province of specialized facilities. Fortunately, virtually every practice can afford to implement technology at the point of care that can drive that optimal care. DLCO measurements are critical information that clinicians can use to provide earlier and more accurate diagnosis that can slow disease progression, enhance quality of life, and provide high-quality, patient-centric care at relatively low cost. They are the very definition of evidence-based practice, and provide extremely high value throughout the continuum of care.
Mapel DW, Dalal AA, Johnson P, Becker L, Hunter AG. A clinical study of COPD severity assessment by primary care physicians and their patients compared with spirometry. Am J Med. 2015;128(6):629-637. doi:10.1016/j.amjmed.2014.12.018 ↩︎
Lutfi MF. The physiological basis and clinical significance of lung volume measurements. Multidiscip Respir Med. 2017;12(1):3. doi:10.1186/s40248-017-0084-5 ↩︎
Ruppel GL. What is the clinical value of lung volumes? Respir Care. 2012;57(1):26-38. doi:10.4187/respcare.01374 ↩︎
Organs and Structures of the Respiratory System | Anatomy and Physiology II. https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/organs-and-structures-of-the-respiratory-system/. Accessed April 8, 2021. ↩︎
Lam-Phuong Nguyen, Richart W. Harper, Samuel Louie. Using and Interpreting Carbon Monoxide Diffusing Capacity (Dlco) Correctly. Consultant. 2016;56(5):440-445. https://www.consultant360.com/articles/using-and-interpreting-carbon-monoxide-diffusing-capacity-dlco-correctly. Accessed April 9, 2021. ↩︎
Doubková M, Švancara J, Svoboda M, et al. EMPIRE Registry, Czech Part: Impact of demographics, pulmonary function and HRCT on survival and clinical course in idiopathic pulmonary fibrosis. Clin Respir J. 2018;12(4):1526-1535. doi:10.1111/crj.12700 ↩︎
Stadler S, Mergenthaler N, Lange TJ. The prognostic value of DLCO and pulmonary blood flow in patients with pulmonary hypertension. Pulm Circ. 2019;9(4). doi:10.1177/2045894019894531 ↩︎
Kacprzak A, Szturmowicz M, Franczuk M, et al. Clinical meaning of low DLCO in idiopathic pulmonary arterial hypertension (IPAH) - Prospective single centre study. In: European Respiratory Journal. Vol 46. European Respiratory Society (ERS); 2015:PA2117. doi:10.1183/13993003.congress-2015.pa2117 ↩︎
Saydain G, Beck KC, Decker PA, Cowl CT, Scanlon PD. Clinical Significance of Elevated Diffusing Capacity. Chest. 2004;125(2):446-452. doi:10.1378/chest.125.2.446 ↩︎
Balasubramanian A, MacIntyre NR, Henderson RJ, et al. Diffusing Capacity of Carbon Monoxide in Assessment of COPD. Chest. 2019;156(6):1111-1119. doi:10.1016/j.chest.2019.06.035 ↩︎
Enright P. Office-based DLCO tests help pulmonologists to make important clinical decisions. Respir Investig. 2016;54(5):305-311. doi:10.1016/j.resinv.2016.03.006 ↩︎
Criner RN, Hatt CR, Galbán CJ, et al. Relationship between diffusion capacity and small airway abnormality in COPDGene. Respir Res. 2019;20(1). doi:10.1186/s12931-019-1237-1 ↩︎