The importance of PFT in long COVID

Much attention has been focused on the ever-rising death toll from the COVID-19 pandemic. Of course, the “light in the darkness” is that thanks to the heroic efforts of physicians, respiratory therapists, nurses, and the rest of the clinical team, most people infected by the virus do, in fact, recover.
In addition, many who get infected don’t even encounter an inpatient care team. These mild COVID-19 cases are managed much like other respiratory infections - with supportive care and other therapies prescribed through an ambulatory care provider. But as we enter the second year of this pandemic and learn more about the SARS-CoV-2 virus, we continue to encounter more and more surprises.
Mild COVID-19 cases #
One of the more recent discoveries is that while those so-called ‘mild’ cases of COVID-19 may not have the dramatic, severe symptoms of cases requiring hospitalization, mild cases may be just as likely to cause insidious damage with long-term health consequences. Just how bad that damage can get is still being investigated, and pulmonary function testing can and should be a part of that investigation.
Just what does ‘mild’ mean? #
First, it’s important to remember that “mild” is more of a relative term than a clinical one. Any COVID-19 case that doesn’t land you in the hospital could be considered mild. But this isn’t necessarily just a case of the sniffles, either. The Centers for Disease Control and Prevention (CDC) lists a raft of symptoms from fever and chills to fatigue and body ache to the shortness of breath that is a hallmark of virtually any respiratory infection.
Anyone who has had a rough case of the flu can tell you that none of those symptoms is particularly pleasant to endure, and even the two weeks in which these mild cases generally resolve could feel like an eternity. However, a new study from the American Thoracic Society (ATS) ominously hints that for some, it may actually be an eternity.
The link between mild cases and ’long COVID’ #
A new study from the American Thoracic Society (ATS) ominously hints that for some, it may actually be an eternity. A team from Ireland found that ongoing fatigue, malaise, and shortness of breath were rather common even two to three months after an initial COVID-19 diagnosis1.
In fact, the study reported that over 60% of the cohort felt they had “not returned to full health” after a median time of 75 days had elapsed from diagnosis to follow-up. And while the study did include some more severe cases, it doesn’t bode well for the mild ones, as the team found none of their measures were associated in any way with the initial severity of the case.
A similar study conducted here in the United States found similar results. 177 people with confirmed COVID-19 were followed for between 3 and 9 months by a team with the University of Washington. They found a slightly lower prevalence of what is now being called ‘long COVID’, with roughly a third of the subjects reporting ongoing symptom burden. However, in this group, they found 14 (8% of the cohort) who had symptoms severe enough to affect their activities of daily living, and nine of these subjects had not even been hospitalized.2
This study also is sure to highlight that while the percentage prevalence may be objectively low, with the now-hundreds of millions of cases worldwide, the potential public health and economic consequences of this level of debilitation could be severe.
The missing component #
The potential burden of long COVID makes it absolutely critical that we understand as much as we can as fast as we can. That motivation makes it somewhat surprising (bordering on baffling) that these two hallmark studies have overlooked a key component in respiratory disease management: pulmonary function testing. The University of Washington study focused on patient-reported outcomes, whereas the Irish group did use a variety of imaging and other diagnostic tests. Yet, they overlooked even basic spirometry.
Notably, despite finding unexpectedly low incidences of fibrosis on CT scans (which the team expected in light of the various reports of dyspnea), there was no follow-up effort to measure any other lung parameter. This is particularly surprising considering an Austrian team published findings last year in the European Respiratory Journal that indicated significant alterations in airflow and diffusion capacity (DLCO) over three months after initial diagnosis3.
In this study, a solid 40% of subjects reported ongoing shortness of breath and other symptoms at the 100-day mark, which could be partially explained by 1) the 22% that had below-predicted FEV1 or FVC measurements, 2) the 21% that had reductions in DLCO, and 3) the 11% who had reduced total lung capacity (TLC).
These are important figures not only because they show the ongoing burden of COVID-19, but they highlight the risks and limitations of more common tests like CT imaging. Even with the best equipment and staff, certain things can be difficult to discern on CT scans, such as differentiating between the resolving inflammation of COVID-19 and the development of permanent fibrotic scar tissue, as the Austrian team highlights in their paper. Post-COVID fibrosis is a growing concern, with some patients even requiring lung transplantation to survive. If clinicians had a tool that could help them identify these patients sooner and begin more effective monitoring and treatment, those extreme solutions might not be necessary. In addition, by better understanding how the post-COVID lung actually works, we will be in a much better position to create community and population health initiatives to make sure long-haul COVID-19 patients get the tools they need to return to full function.
The role of PFT during COVID-19 #
Fortunately, such a tool already exists; we just don’t use it enough. Pulmonary function testing is an ideal tool for assessing the physiological impact of a virus that largely attacks the cardiopulmonary system. The technology behind measuring airflow, lung volumes, and the ability for oxygen and carbon dioxide to transfer between the alveoli and the bloodstream are well established, and facilities to perform these tests are found around the country.
The current PFT infrastructure isn’t enough to fully respond to the challenges posed by COVID-19. First and foremost, there are not enough PFT labs around the country, and the ones that are available still experiencing disruptions. Due to the nature of PFTs, it is often thought that they place clinicians and patients alike at additional exposure risk.
How to effectively implement PFT for long COVID #
A better solution is clearly to introduce pulmonary function testing at the point of care, but this has historically been viewed as out of reach of the ‘average’ office practice due to the cumbersome form factor and complex operation (not to mention significant cost investment) for a full PFT suite. It seems likely that lack of equipment could have played a role in the missing PFT data from the two long COVID articles discussed earlier.
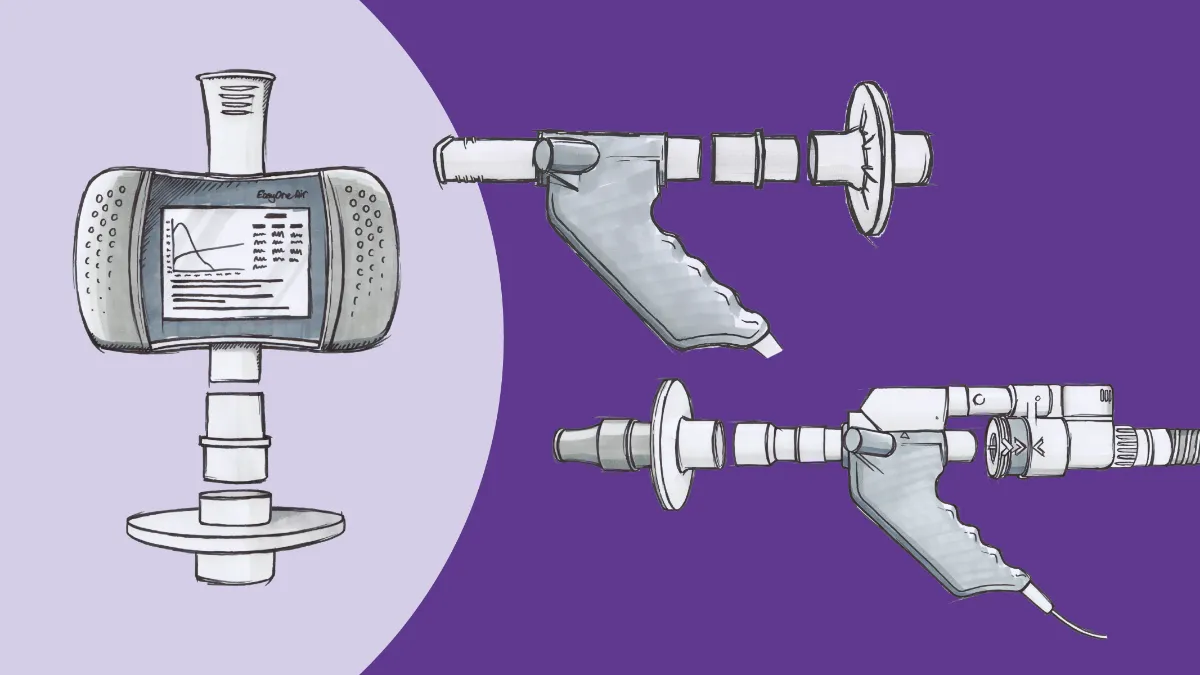
Fortunately, there is a solution here. Modern technology has reduced the size and expense of this equipment to bring it within reach of every practice. The ndd EasyOne© Air is an economical, handheld solution that empowers clinics and offices of any size to quickly start a spirometry program and test patients where they are instead of where you want them to go.
The benefits of spirometry at point of care #
Moving spirometry to the point of care not only makes things easier on your patients, but has the potential to massively increase the set of data available for research in several different aspects. Regular lung ‘checkups’ have usually only consisted of some auscultation along with a handful of interview questions.
As a result, diagnosis of conditions like COPD is routinely delayed.Delayed diagnoses have been associated with increased healthcare costs and worsened outcomes, and some studies have suggested that this is an area where primary care providers can make substantial contributions to improving the quality of the overall healthcare system.4
This is not a heavy lift, either. The unique ultrasonic TrueFlow™ technology at the heart of every EasyOne Air requires no calibration, meaning your staff doesn’t have to spend their time wrestling with syringes; they can simply grab the device, enter the patient’s data on the color touchscreen, and get to work.
The EasyOne Air can also be used with a computer USB or Bluetooth, allowing for additional incentive and coaching screens to make every test consistent and valid. Integration with major EMR systems allows for rapid clinical decision-making and care coordination, as well as simplified data collection for research.
That means with one device, you can easily establish baseline airflow status for every patient, even those potentially at risk for a chronic respiratory condition (including your COVID-19 population), and keep an eye out for anomalies before they become noticeable symptoms.
The benefits of complete PFT at point of care #
ndd also has a similarly practical solution for DLCO testing. The EasyOne Pro™ line eliminates the need for the expensive, bulky ‘body box’ plethysmograph usually associated with measuring DLCO, thus bringing DLCO capability to any desktop or cart in your office. This means, once again, virtually any practice now has the power to screen for potential COVID-19 sequelae (like pulmonary fibrosis) much earlier than before.
Thanks to the built-in TrueCheck™ technology which automatically calibrates the gas analyzer before each test, the EasyOne Pro is proven and peer-reviewed to deliver accurate, consistent measurements with very little user maintenance or service requirements, allowing your staff to focus on the patient, not yet another screen.5 The reliability of this technology also ensures repeatability over time, essential for discovering trends in individual lung health. And, the EasyOne Pro also integrates all the spirometry capability of the EasyOne Air.
Mitigating the risk of infection and increasing revenue #
With either solution, infection control procedures are also quite simple. All components that the user’s exhaled gas comes into contact with are disposable. Inline and ultraviolet sanitation options are available to protect your staff and other patients during the pandemic and after.
The exteriors of all ndd devices are easily wiped down and sanitized, minimizing disruptions in patient flow due to ‘terminal’ cleanings. With older PFT body boxes, that can take 30 minutes or more. Both sets of tests are already reimbursable through Medicare, Medicaid, and private insurance as well, enabling not only rapid return on investment but an actual revenue stream.
What next…? #
The COVID-19 pandemic has revealed many structural problems and inefficiencies throughout the healthcare system. One of those inefficiencies is the uneven density of pulmonary function testing capacity across the country.
There is a clear need to better understand and monitor the long-term effects of COVID-19, and that starts with increasing PFT availability by adding testing equipment wherever possible. With 27 million people in the U.S. alone having recovered from COVID-19, we can no longer overlook spirometry or DLCO in the monitoring of patients going forward. While we still have much to learn about this virus and its effects, we already know these tools are far too important to leave on the bench.
Townsend L, Dowds J, O’Brien K, et al. Persistent Poor Health Post-COVID-19 Is Not Associated with Respiratory Complications or Initial Disease Severity. Ann Am Thorac Soc. Published online 2021. doi:10.1513/annalsats.202009-1175oc ↩︎
Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open. 2021;4(2):e210830. doi:10.1001/jamanetworkopen.2021.0830 ↩︎
Sonnweber T, Sahanic S, Pizzini A, et al. Cardiopulmonary recovery after COVID-19 - an observational prospective multi-center trial. Eur Respir J. Published online December 10, 2020. doi:10.1183/13993003.03481-2020 ↩︎
Larsson K, Janson C, Ställberg B, et al. Impact of COPD diagnosis timing on clinical and economic outcomes: The ARCTIC observational cohort study. Int J COPD. 2019;14:995-1008. doi:10.2147/COPD.S195382 ↩︎
Gochicoa-Rangel L, Pérez-Padilla R, Vázquez-García JC, et al. Long-term stability of a portable carbon monoxide single-breath diffusing capacity instrument. Respir Care. 2017;62(2):231-235. doi:10.4187/respcare.04983 ↩︎