DLCO in preoperative surgery

Pulmonary resections are high-risk surgeries, even for otherwise healthy individuals. Preoperative assessment is crucial in anesthesia management to focus on pulmonary, cardiac, and infectious risk factors.
Patients experience a decline in perfusion and lung ventilation during surgery, which puts them at an elevated risk for post-surgical complications. Patients who smoke, have lung disease, or other underlying health conditions, are at increased risk for postoperative complications.
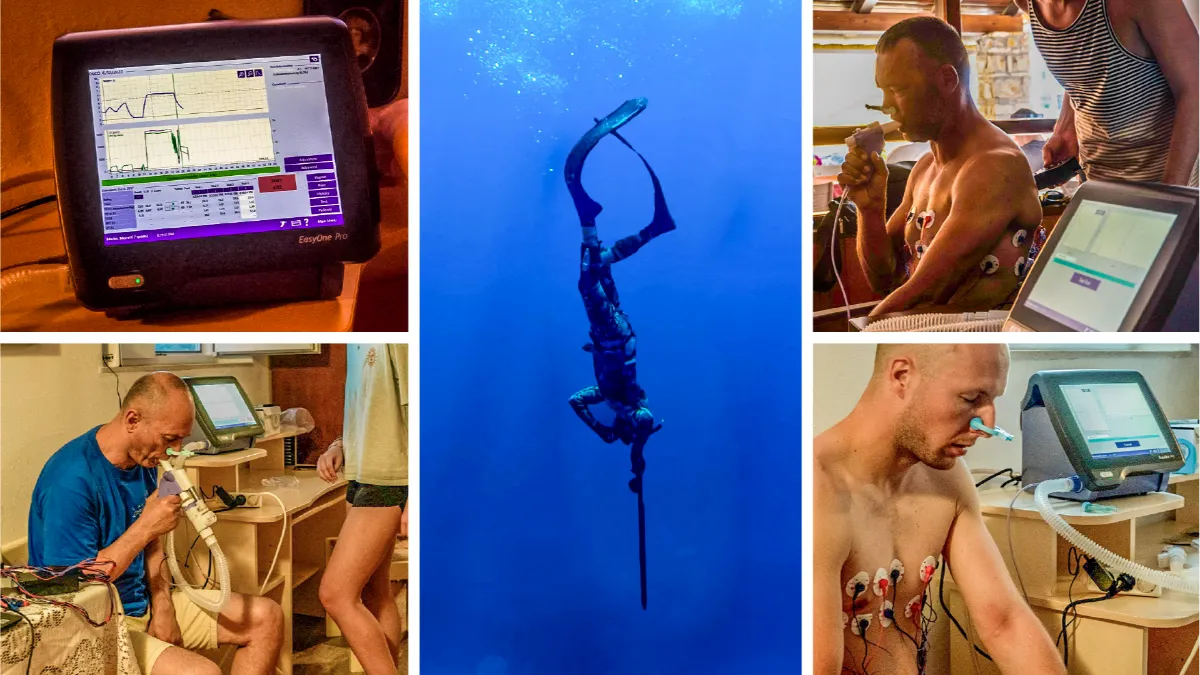
To lower postoperative risks for these patients, clinicians perform preoperative baseline tests, which include pulmonary function testing (PFT).
Why do a preoperative PFT evaluation? #
Pulmonary function tests obtain parameters that help identify postoperative risks, allowing physicians and healthcare providers to implement measures to prepare patients for high-risk surgery.
While lung resections are risky procedures , patients with comorbidities are at an increased risk. Existing comorbidities, combined with anesthesia, increase the risk of post-surgical complications. In addition, certain drugs that suppress the respiratory system, combined with splinting, pain, and a weakened diaphragm, reduce lung volumes and the ability to mobilize airway secretions. These factors eventually lead to atelectasis (a collapse in part or all of the lung), low blood-oxygen levels, or respiratory infections.
Even in otherwise healthy individuals, physiologic changes occur in the respiratory system in all patients undergoing surgical and anesthetic procedures. These changes may lead to 1complications1, such as:
- Lung infections
- Prolonged mechanical ventilation
- Carbon dioxide (CO2) retention
- Bronchospasm
- Atelectasis
- Chronic lung disease exacerbation
- Cardiac arrhythmias
- Myocardial infarctions
- Pulmonary embolisms
- Death
Preoperative PFT evaluations give clinicians a baseline assessment, allowing them to determine postoperative outcomes and adjust patient care for optimal outcomes.
The importance of PFT parameters #
Preoperative PFT parameters are crucial for lung resections because of the procedure’s high risk. Depending on the degree of the lung resection, an estimated 30 percent of patients develop cardiopulmonary complications, with 30-day mortality between 0.6 and 5 percent.2
Predicting postoperative pulmonary function parameters with diffusion capacity testing, lung volume testing, and spirometry identifies patients with risk factors for complications after lung resection.3
In addition to determining baseline parameters in patients with lung disease, PFT parameters also detect undiagnosed lung disease and damage, which is one reason why all patients benefit from PFT evaluations, regardless of age or underlying medical conditions.
It’s vital to determine whether patients will tolerate one-lung ventilation intraoperatively and have sufficient pulmonary reserve after the operation. Establishing risk factors allows healthcare providers to implement measures, preparing these patients for the operation.
DLCO in preoperative care #
DLCO testing measures the diffusion capacity of the lungs, which determines how well the lungs transfer gases from inhaled air to the pulmonary capillaries’ red blood cells. It effectively detects lung damage and lung diseases.
DLCO is a necessary preoperative test, but physicians often rely on spirometry tests, like FEV1 (forced expiratory volume in the first second of exhalation), to determine postoperative risk factors. Diffusing capacity of the lungs for carbon monoxide (DLCO) is often unused in patients with normal spirometry results due to a perceived lack of value. However, research shows no correlation between FEV1 and DLCO when determining postoperative risk factors, and the use of DLCO testing would be beneficial.4
DLCO testing offers powerful predictions for determining complications following lung resection.
Numerous studies show that DLCO offers a more vital prediction of postoperative complications than FEV1, even in patients with normal spirometry.5 Further research determined that using DLCO independently determines long-term survival after lung resection in patients with lung cancer.6
DLCO is a crucial preoperative test that providers can use with FEV1 to offer a more vital determination of postoperative risk factors. Visit here to learn more about DLCO testing.