Point of care pulmonary function testing: Important now, more than ever

As the relentless waves of the COVID-19 pandemic continue to wash over the world, much attention has been focused on the idea of hospital bed shortages. As cases strain hospital systems everywhere, the most-commonly reported metrics one hears have to do with beds; how many ICU beds left, how many emergency beds, how many beds overall. While it is of course critical to understand how much physical space remains to care for patients sick enough to require admission, bed numbers only tell one part of the story. After all, even once safely ensconced in a hospital bed, someone admitted to the hospital still needs someone to provide actual care. With a respiratory pandemic like COVID-19, that often means a respiratory therapist (RT), there to provide oxygen therapy, aerosol medications, or mechanical ventilation support is needed.
The need for respiratory professionals #
Prior to the advent of COVID-19, a shortage of respiratory therapists was brewing. According to a survey of respiratory care thought leaders commissioned by the American Association for Respiratory Care (AARC), almost 90% felt that they were either already in the midst of a local shortage of RTs or one was imminent.1 In the same survey, those leaders felt that a major driver of this shortage was an increase in the need for high-quality respiratory diagnostics across the continuum of care. The COVID-19 pandemic has only exacerbated both issues; RTs have not been immune to the burnout-related exodus the overall healthcare system has been experiencing, and the looming specter of long COVID has made pulmonary function testing more important than ever.
A ‘perfect storm’ #
This may not seem like a problem with immediate impact in the outpatient world, but these issues have created a ‘perfect storm’ that resonates well beyond the hospital walls. This blog has covered the safe operation of pulmonary function tests in various settings several times, and while those principles haven’t really changed with the advent of the Delta and Omicron variants of SARS-CoV-2, PFT labs are faced with a similar challenge as inpatient unit leaders and bed utilization managers: Not enough staff. Surging inpatient demand for respiratory therapists has led to integrated healthcare systems reassigning RTs (and their irreplaceable skillsets) from ambulatory roles like pulmonary rehabilitation and diagnostics to critical care bedsides. We saw this at the beginning of the pandemic of course, but unfortunately it seems past is indeed prologue and these transfers are needed once again. This has the potential to lead to new delays in testing just as PFT labs were finally starting to catch up to the backlogs experienced in mid-2020.
Point of care pulmonary function testing #
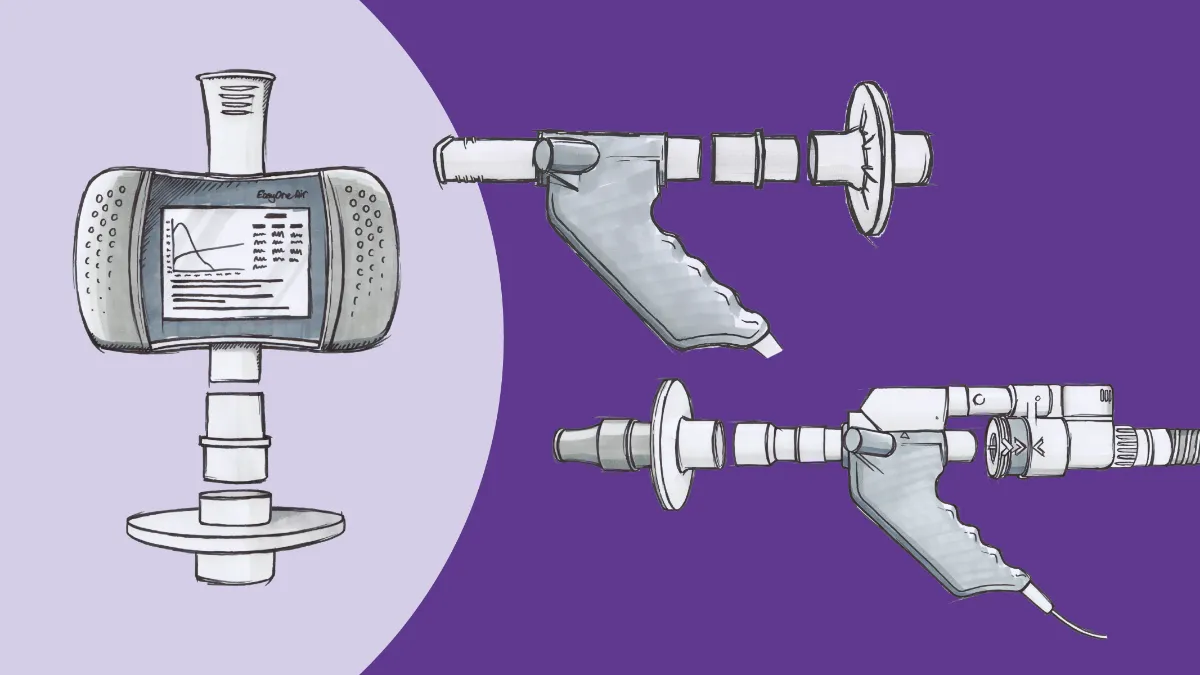
However, all is not lost. Pulmonary function testing is no longer solely the domain of specialized facilities or even hospitals. Clinics and individual practices now have the ability to perform the full range of testing directly at the point of care, saving time and improving efficiency. While the ideal staffing model would still include a trained and credentialed pulmonary function technologist, modern testing equipment is user-friendly enough to facilitate the training of virtually any staff member on basic operations. For example, the EasyOne Air portable spirometer has a built-in display with visual and audio prompts and a variety of interpretation standards that integrate well with any practice’s records. Attaching the EasyOne Air to a computer provides access to several animated incentive screens, providing immediate feedback concerning effort and technique to both the technician and the test subject. And preliminary interpretations are provided based on American Thoracic Society and European Respiratory Society algorithms, giving you the context to make immediate therapy decisions. The entire EasyOne line has been designed for both safety and ease of use, with integrated TrueFlow™ technology eliminating the need for cumbersome and time-consuming calibration processes, and bacterial/viral filters available to protect your staff and your patients.
Safety is, of course, another tremendous advantage of point-of-care pulmonary function testing. Sadly, many people with chronic respiratory conditions are tested relatively late in their disease progression. This means that they’re already at enhanced risk for respiratory infections, particularly COVID-19. Despite the safety precautions most PFT labs have in place, the wisest course of action to reduce risk is always to minimize potential exposures, which means reducing the number of places your patients must visit. Devices like those in the EasyOne PFT product line make it, well, easy to set up a ‘one-stop shopping’ approach reducing potential exposures. Point-of-care pulmonary function testing often makes logistics and scheduling much easier for your patients as well, since they are no longer forced to arrange additional transportation (another potential infection vector), take time off work, or scramble to find an in-network facility with available appointments.
Finally, point-of-care pulmonary function testing also makes it easier on you, the clinician. The advent of the electronic medical record was supposed to herald a new era of simple communication and interconnectivity, but unfortunately reality has not quite caught up with that ideal. Certainly, offices that share an affiliation can (usually) share records fairly easily, but what about independent practices? What about rural practices, some of whom are still heavily reliant on paper and faxes? Communication breakdowns in these settings can delay proper diagnosis even longer, preventing patients from accessing the therapies that can have a tremendous difference in their quality of life. However, by providing on-site testing, clinicians get results virtually in real-time, ensuring your patients get the most appropriate treatments literally as soon as possible. Developing a testing program can also provide an additional revenue stream, with relatively low capital investment and reasonable reimbursement through Medicare and private payers.
What’s next? #
Healthcare systems around the world have been adapting almost continuously since the start of the COVID-19 pandemic. Some of those adaptations have been because the virus has introduced new challenges, but many others have been because the pandemic simply shone a light on deficiencies and barriers that have long been present. The need for point-of-care pulmonary function testing falls mostly into the latter category, with the advantages of knowing a patient’s pulmonary status immediately (and without the risks of communication failure or becoming lost to follow-up) now more prominent in the minds of many. The need for point-of-care pulmonary function testing will only increase in the aftermath of the COVID-19 pandemic, regardless of how many variants we encounter. Whether it is relieving staffing pressures, reducing a patient’s logistical burden, or simply facilitating a clinical decision, on-site pulmonary function testing is clearly a winning strategy for clinics and practices of every size.
Help Us Address the Shortage - Respiratory Therapist Campaign. Accessed December 29, 2021. https://www.morerts.com/growing-need/ ↩︎