Increased utilization of spirometry: The solution to both mis- and underdiagnosed lung conditions

Spirometry is crucial for accurately diagnosing lung conditions #
Spirometry is a common pulmonary function test used to evaluate the health of a person’s lungs. There are many parameters generated from a spirometry test. Three are primarily used in the clinic: Forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), and the ratio of FEV1 to FVC (FEV1/FVC).1 Spirometry is used to deduce whether a person first demonstrates a possibility of lung disease. Based on the FVC, FEV1, and FEV1/FVC values, trained clinicians can then discern whether the patient has restrictive or obstructive patterns of lung disease.1 Spirometry, like many tools, is not the only instrument clinicians should use to diagnose a patient presenting with symptoms such as shortness of breath.2 Instead, spirometry should be used as a first line of inquiry intended to guide next steps.
Spirometry is an essential component for diagnosing lung diseases. The test is used in the diagnosis and management of chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, pulmonary fibrosis, emphysema, bronchiectasis, and even some forms of lung cancer, all conditions which present with different constellations of symptoms and spirometric signatures.3 Spirometry is even required by Occupational Safety and Health Administration (OSHA) to screen workers for job assignments and monitor workers for potential exposure-related health effects.
There is a crisis of under- and misdiagnosed lung conditions #
While the journey of patients managing their chronic, progressive lung condition becomes dramatically different once they receive a diagnosis, that’s not where it begins. Some patients might not even begin with spirometry. For many patients, their journey begins years prior to their diagnosis, many of whom are seeing multiple specialists and even receiving multiple diagnoses — or never receiving one — before getting an accurate one. There are ramifications related to delayed diagnoses, burdening the patient’s body and their mind as they navigate appointments, tests, and therapies. One study found that school-aged children with undiagnosed asthma had more than seven absences from school in the previous year compared to their healthy peers.4 Another study found adults with undiagnosed asthma had poorer quality of life than their peers.5 It’s only reasonable to suspect that these consequences are paralleled in other conditions, underscoring the importance of adequately diagnosing patients.
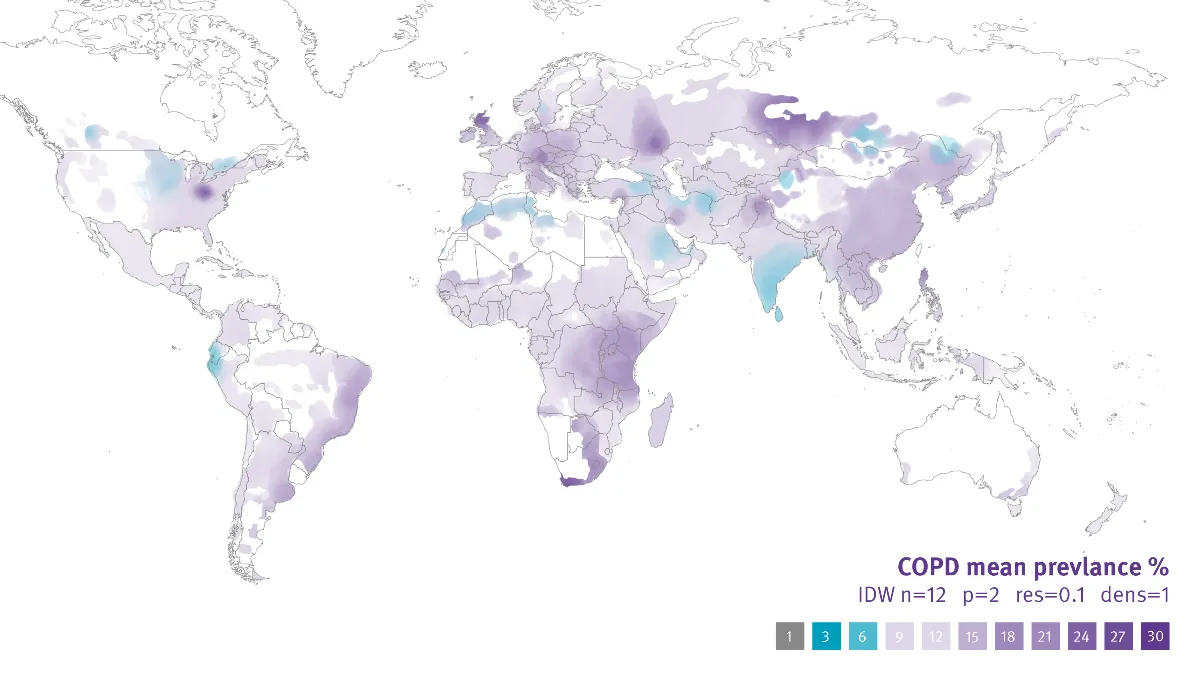
Unfortunately, a great deal of people live with undiagnosed or misdiagnosed lung diseases, with estimates ranging up to 95% of global cases of COPD remaining undiagnosed.6 This extremely high figure raises concern about how many people are living with COPD without receiving adequate treatment. It is also concerning that the prevalence of conditions is not truly known due to a large percentage of true cases not counted as well as an overcounting because of misdiagnoses. Positively, many studies point to the same culprit for both issues: An underutilization of spirometry. 7
Spirometry underutilization is widespread, both geographically and in the clinic: Spirometry is underutilized in primary and specialized care and in hospitals in at least the United States, Malaysia, Spain, and Italy.8 The authors of one paper investigating the significance of this problem capture the magnitude of this problem: “Not performing spirometry is the strongest predictor for an incorrect diagnosis of COPD.”6
Why is spirometry so underutilized and how can we increase spirometry utilization? #
Even though spirometry is well-established as the standard to confirm diagnoses for many lung diseases, logistical and systemic issues such as lack of access to resources, expensive spirometry devices, general confusion, and conflicting guidance within the field are just some of the barriers to increased utilization of spirometry.9Additionally, older patients, those who are not receiving pulmonary care, and patients with fewer comorbidities are less likely to perform spirometry.10
Fortunately, with the advent of portable, easy to use, point of care devices like EasyOne Air, access to accurate spirometry devices is becoming less of an issue. Still, other barriers remain and must be resolved. Global awareness of the significance of spirometry must be covered more loudly and broadly than it is in the present alongside more consistency in guidance documents. Improved education is another part of the solution too, with senior doctors educating junior physicians on the importance of using spirometry as part of a systematic diagnostic approach. Studies in the US and Italy have corroborated findings that with increased training and education and the routine use of spirometry, the detection of currently significantly under-diagnosed airway obstruction in hospitalized patients would improve.11
Spirometry underutilization is a rampant global issue leading to legions of misdiagnosed and undiagnosed patients. With increased access to portable devices, increased and improved education and teaching of medical professionals, and with better awareness of how spirometry is required in the diagnosis of many lung conditions, there will be a profound shift in the way lung conditions are diagnosed and treated around the world.
Haynes JM. Basic spirometry testing and interpretation for the primary care provider. Can J Respir Ther CJRT Rev Can Thérapie Respir RCTR. 2018;54(4):10.29390/cjrt-2018-017. doi:10.29390/cjrt-2018-017 ↩︎ ↩︎
What Kind of Lung Function Tests Are There and What Do They Involve? Institute for Quality and Efficiency in Health Care (IQWiG); 2016. Accessed February 14, 2023. https://www.ncbi.nlm.nih.gov/books/NBK355303/ ↩︎
(3) Johns DP, Walters JAE, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis. 2014;6(11):1557-1569. doi:10.3978/j.issn.2072-1439.2014.08.18
(4) Amariei DE, Dodia N, Deepak J, et al. Combined Pulmonary Fibrosis and Emphysema: Pulmonary Function Testing and a Pathophysiology Perspective. Med Kaunas Lith. 2019;55(9):580. doi:10.3390/medicina55090580
(5) Zhai T, Li Y, Brown R, Lanuti M, Gainor JF, Christiani DC. Spirometry at diagnosis and overall survival in non-small cell lung cancer patients. Cancer Med. 2022;11(24):4796-4805. doi:10.1002/cam4.4808
(6) Bulcun E, Arslan M, Ekici A, Ekici M. Quality of Life and Bronchial Hyper-Responsiveness in Subjects With Bronchiectasis: Validation of the Seattle Obstructive Lung Disease Questionnaire in Bronchiectasis. Respir Care. 2015;60(11):1616-1623. doi:10.4187/respcare.03906 ↩︎van Gent R, van Essen LEM, Rovers MM, Kimpen JLL, van der Ent CK, de Meer G. Quality of life in children with undiagnosed and diagnosed asthma. Eur J Pediatr. 2007;166(8):843-848. doi:10.1007/s00431-006-0358-y ↩︎
Adams RJ, Wilson DH, Appleton S, et al. Underdiagnosed asthma in South Australia. Thorax. 2003;58(10):846-850. doi:10.1136/thorax.58.10.846 ↩︎
Ho T, Cusack RP, Chaudhary N, Satia I, Kurmi OP. Under- and over-diagnosis of COPD: a global perspective. Breathe. 2019;15(1):24-35. doi:10.1183/20734735.0346-2018 ↩︎ ↩︎
(3) Johns DP, Walters JAE, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis. 2014;6(11):1557-1569. doi:10.3978/j.issn.2072-1439.2014.08.18
(9) Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and Overdiagnosis of Asthma. Am J Respir Crit Care Med. 2018;198(8):1012-1020. doi:10.1164/rccm.201804-0682CI
(10) Ho T, Cusack RP, Chaudhary N, Satia I, Kurmi OP. Under- and over-diagnosis of COPD: a global perspective. Breathe. 2019;15(1):24-35. doi:10.1183/20734735.0346-2018
(11) Baldomero AK, Kunisaki KM, Bangerter A, et al. Beyond Access: Factors Associated With Spirometry Underutilization Among Patients With a Diagnosis of COPD in Urban Tertiary Care Centers. Chronic Obstr Pulm Dis Miami Fla. 2022;9(4):538-548. doi:10.15326/jcopdf.2022.0303
(12) Roberts NJ, Smith SF, Partridge MR. Why is spirometry underused in the diagnosis of the breathless patient: a qualitative study. BMC Pulm Med. 2011;11(1):37. doi:10.1186/1471-2466-11-37
(13) Volkova NB, Kodani A, Hilario D, Munyaradzi SM, Peterson MW. Spirometry utilization after hospitalization for patients with chronic obstructive pulmonary disease exacerbations. Am J Med Qual Off J Am Coll Med Qual. 2009;24(1):61-66. doi:10.1177/1062860608326417
(14) Moore PL. Practice management and chronic obstructive pulmonary disease in primary care. Am J Med. 2007;120(8 Suppl 1):S23-27. doi:10.1016/j.amjmed.2007.04.009
(15) Lusuardi M, Garuti G, Massobrio M, Spagnolatti L, Bendinelli S. Heart and lungs in COPD. Close friends in real life–separate in daily medical practice? Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2008;69(1):11-17. doi:10.4081/monaldi.2008.406
(16) Petty TL. Benefits of and barriers to the widespread use of spirometry. Curr Opin Pulm Med. 2005;11(2):115-120. doi:10.1097/01.mcp.0000150948.13034.78
(17) Fauzi AR. Knowledge and practice of medical doctors on chronic obstructive pulmonary disease: a preliminary survey from a state hospital. Med J Malaysia. 2003;58(2):205-212.
(18) Alvarez Luque I, Flor Escriche X, Rodríguez Mas M, et al. [Do we forget asthma as a chronic illness in our primary care consultations?]. Aten Primaria. 2004;33(7):381-386. doi:10.1016/s0212-6567(04)78890-3
(19) Zaas D, Wise R, Wiener C, Longcope Spirometry Invetigation Team. Airway obstruction is common but unsuspected in patients admitted to a general medicine service. Chest. 2004;125(1):106-111. doi:10.1378/chest.125.1.106 ↩︎(12) Roberts NJ, Smith SF, Partridge MR. Why is spirometry underused in the diagnosis of the breathless patient: a qualitative study. BMC Pulm Med. 2011;11(1):37. doi:10.1186/1471-2466-11-37
(13) Volkova NB, Kodani A, Hilario D, Munyaradzi SM, Peterson MW. Spirometry utilization after hospitalization for patients with chronic obstructive pulmonary disease exacerbations. Am J Med Qual Off J Am Coll Med Qual. 2009;24(1):61-66. doi:10.1177/1062860608326417
(15) Lusuardi M, Garuti G, Massobrio M, Spagnolatti L, Bendinelli S. Heart and lungs in COPD. Close friends in real life–separate in daily medical practice? Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2008;69(1):11-17. doi:10.4081/monaldi.2008.406
(17) Fauzi AR. Knowledge and practice of medical doctors on chronic obstructive pulmonary disease: a preliminary survey from a state hospital. Med J Malaysia. 2003;58(2):205-212.
(18) Alvarez Luque I, Flor Escriche X, Rodríguez Mas M, et al. [Do we forget asthma as a chronic illness in our primary care consultations?]. Aten Primaria. 2004;33(7):381-386. doi:10.1016/s0212-6567(04)78890-3
(19) Zaas D, Wise R, Wiener C, Longcope Spirometry Invetigation Team. Airway obstruction is common but unsuspected in patients admitted to a general medicine service. Chest. 2004;125(1):106-111. doi:10.1378/chest.125.1.106 ↩︎(9) Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and Overdiagnosis of Asthma. Am J Respir Crit Care Med. 2018;198(8):1012-1020. doi:10.1164/rccm.201804-0682CI
(14) Moore PL. Practice management and chronic obstructive pulmonary disease in primary care. Am J Med. 2007;120(8 Suppl 1):S23-27. doi:10.1016/j.amjmed.2007.04.009
(16) Petty TL. Benefits of and barriers to the widespread use of spirometry. Curr Opin Pulm Med. 2005;11(2):115-120. doi:10.1097/01.mcp.0000150948.13034.78
(20) Fromer L, Cooper CB. A review of the GOLD guidelines for the diagnosis and treatment of patients with COPD. Int J Clin Pract. 2008;62(8):1219-1236. doi:10.1111/j.1742-1241.2008.01807.x
(21) Walters JA, Hansen EC, Johns DP, Blizzard EL, Walters EH, Wood-Baker R. A mixed methods study to compare models of spirometry delivery in primary care for patients at risk of COPD. Thorax. 2008;63(5):408-414. doi:10.1136/thx.2007.082859
(22) Wickstrom GC, Kolar MM, Keyserling TC, et al. Confidence of graduating internal medicine residents to perform ambulatory procedures. J Gen Intern Med. 2000;15(6):361-365. doi:10.1046/j.1525-1497.2000.04118.x
(23) Cranston JM, Crockett AJ, Moss JR, Pegram RW, Stocks NP. Models of chronic disease management in primary care for patients with mild-to-moderate asthma or COPD: a narrative review. Med J Aust. 2008;188(S8):S50-52. doi:10.5694/j.1326-5377.2008.tb01744.x
(24) Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD Resource Network Needs Assessment Survey. Am J Med. 2005;118(12):1415. doi:10.1016/j.amjmed.2005.07.059 ↩︎Baldomero AK, Kunisaki KM, Bangerter A, et al. Beyond Access: Factors Associated With Spirometry Underutilization Among Patients With a Diagnosis of COPD in Urban Tertiary Care Centers. Chronic Obstr Pulm Dis Miami Fla. 2022;9(4):538-548. doi:10.15326/jcopdf.2022.030 ↩︎
COPD. Close friends in real life–separate in daily medical practice? Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2008;69(1):11-17. doi:10.4081/monaldi.2008.406
Zaas D, Wise R, Wiener C, Longcope Spirometry Investigation Team. Airway obstruction is common but unsuspected in patients admitted to a general medicine service. Chest. 2004;125(1):106-111. doi:10.1378/chest.125.1.106 ↩︎
Written by

Tré LaRosa
Tré LaRosa is a consultant, scientist, and writer in the Washington, DC area with extensive experience working in research (basic, translational, and clinical) and on patient-reported outcomes. He has also written extensively on neuroscience, pulmonology, and respiratory conditions, including from the patient perspective. He enjoys learning, reading, writing, spending time outdoors, and telling everybody about his mini golden retriever, Duncan.