How to interpret spirometry results: A simple guide
Understanding spirometry interpretation is essential for accurately assessing lung function and distinguishing obstructive from restrictive patterns. The guide explains key parameters, along with the importance of patient coaching, acceptable test criteria, and repeatability standards when reading spirometry results. Proper technique and adherence to American Thoracic Society / European Respiratory Society guidelines ensure reliable measurements that support accurate diagnosis and treatment decisions, strengthening clinical confidence and improving the accuracy of spirometry interpretation in everyday practice.
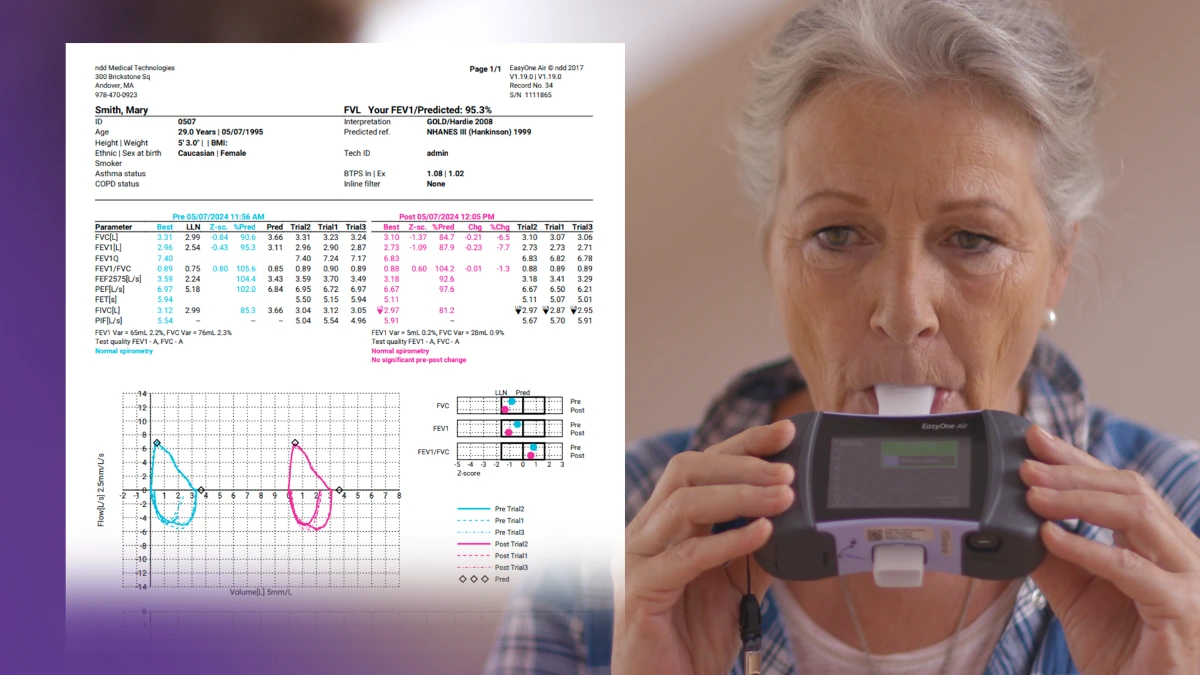
Spirometry is a common method used to assess lung function. It can help differentiate and diagnose obstructive and restrictive lung disease, monitor disease progression, and evaluate the effectiveness of a current treatment plan.
Pulmonary function test basics: Spirometry interpretation #
Spirometry results depend on patient effort and accurate coaching. Pulmonary function tests such as spirometry can be anxiety-inducing and physically stressful for patients. It’s essential to coach patients with graphic instructions before the test and verbal cues throughout the spirometry test to achieve maximal effort.1 Verbal encouragement shouldn’t be underestimated; it makes a big difference, particularly toward the end of the maneuver. In fact, good coaching makes people feel more comfortable and boosts confidence.2
Spirometry must be performed correctly for the results to be interpretable. There are several errors that can lead to unreliable results:
- Sub-maximal inhalation
- Slight hesitation when blowing out at the start of the initial exhalation
- Coughing in the first second
- Failure to completely exhale
- Exhalation speed is reduced due to mouthpiece blockage by tongue, teeth, or biting.
The American Thoracic Society (ATS) and European Respiratory Society (ERS)3 developed criteria to objectively assess whether a patient performed spirometry in an acceptable and usable way. These criteria enable clinicians to know that the measured FEV1 and FVC can be relied upon for clinical decision-making. The table below shows the necessary criteria for each category, divided by FEV1 and FVC.
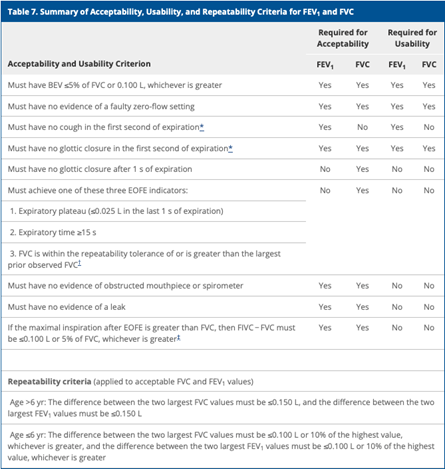
Table 1: Summary of Acceptability, Usability, and Repeatability Criteria for FEV1 and FVC per ATS/ERS guidelines.4
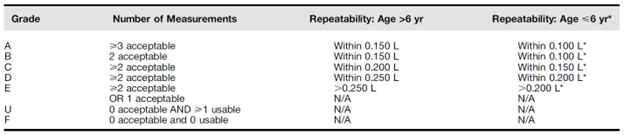
In addition to acceptability and usability, an accurate measurement should also have consistent (repeatable) results for both FVC and FEV1.4 For results to be considered repeatable for people older than six years old, the difference between the largest and second largest values for FVC and FEV1 should be within 0.15 liters (150 ml).4 Up to a maximum of eight additional breathing maneuvers can be attempted to meet the criteria for validation.
The table below represents the 2019 ATS/ERS grading system considering acceptability and repeatability.4
Spirometry parameters: What do the results mean? #
Normal parameters for a spirometry test vary from person to person and depend on age, height, ancestral grouping, and biological sex.5
Forced vital capacity (FVC) is the maximum volume of air a patient can exhale when blowing out as hard and fast as possible. The FVC measurement will be low when a patient can’t inhale deeply or exhale completely. An abnormal FVC measurement could be due to restrictive or obstructive disease, so other spirometry measurements must factor in to determine which type of lung disease is present.
Forced expiratory volume (FEV1) is the volume of air a patient can force out of the lungs in one second. FEV1 helps to evaluate the severity of pulmonary disease. An FEV1 reading below the normal parameter shows a possible breathing obstruction.
FEV1/FVC ratio helps differentiate whether restrictive or obstructive lung disease exists. The FEV1/FVC ratio represents the percentage of lung capacity exhaled in one second.
Technical standards from ERS/ATS classify lung function impairment for all spirometric indices according to z-score.5 Z-scores, as opposed to percent predicted, are now recommended as they describe the number of standard deviations away from predicted value.6
- Z-scores > -1.645 are normal
- Z-scores between -1.65 and -2.5 are considered mild lung function impairment.
- Z-scores between -2.51 and -4 are considered moderate lung function impairment.
- Z-scores < -4.1 are considered severe lung function impairment.
EasyOne spirometry machines—tailored solutions for every practice.
Explore our spirometry machines
Interpreting obstructive versus restrictive lung disease with spirometry #
Measuring FEV1 or FVC alone cannot assess whether a patient has an obstructive or restrictive lung defect. The FEV1/FVC ratio is necessary to determine which problem is present. A patient with obstructive disease may not be able to achieve a normal FEV1 compared to FVC. In contrast, a patient with a restrictive disease may not reach an adequate FVC, but the FEV1/FVC ratio may be normal to slightly elevated.7
Obstruction #
When the FEV1/FVC ratio is less than the lower limit of the normal value for the patient, there could be an obstructive defect. Patients with obstructive disorders cannot exhale adequate volumes of air quickly because of decreased airway diameter. The decrease in diameter resulting in obstruction is often caused by inflammation, mucus plugging, or smooth muscle contraction.
Parameters indicative of an obstructive defect include:7
- Reduced FEV1
- Normal (or reduced) FVC
- Reduced FEV1/FVC ratio
- Normal or reduced VC
- Concave flow-volume loop
Common obstructive lung conditions include asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis.
Restriction #
A reduced FVC with a normal to elevated FEV1/FVC ratio can indicate a restrictive defect. Patients with restrictive lung disease are unable to fully inflate their lungs with air.
Parameters indicative of a restrictive pattern:7
- Slightly reduced or normal FEV1
- Reduced FVC
- Normal-to-high FEV1/FEV ratio
- Possible high PEF
Lung conditions resulting in restrictive defects include idiopathic pulmonary fibrosis, neuromuscular disorders, pulmonary edema, and sarcoidosis.
Spirometry is a crucial tool for treating pulmonary conditions #
Spirometry is a vital test for assessing, diagnosing, and managing lung disease. It’s crucial to obtain accurate measurements for precise diagnosis to manage lung disease better and help impact patient outcomes.
Disclaimer:
ndd Medical Technologies is a medical device manufacturer and does not offer medical advice.
This content is intended for informational purposes only. Always consult a doctor or qualified healthcare provider regarding any questions you may have regarding your spirometry results.
Cheung HJ, Cheung L. Coaching patients during pulmonary function testing: A practical guide. Can J Respir Ther CJRT Rev Can Thérapie Respir RCTR. 2015;51(3):65-68. ↩︎
Johnson B, Steenbruggen I, Graham BL, Coleman C. Improving spirometry testing by understanding patient preferences. ERJ Open Res. 2021;7(1):00712. doi:10.1183/23120541.00712-2020 ↩︎
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-338. doi:10.1183/09031936.05.00034805 ↩︎
Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70-e88. doi:10.1164/rccm.201908-1590ST ↩︎ ↩︎ ↩︎ ↩︎
Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1). doi:10.1183/13993003.01499-2021 ↩︎ ↩︎
Ong-Salvador R, Laveneziana P, Jongh F de. ERS/ATS Global Lung Function Initiative normal values and classifying severity based on z-scores instead of per cent predicted. Breathe. 2024;20(3). doi:10.1183/20734735.0227-2023 ↩︎
Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1). doi:10.1183/13993003.01499-2021 ↩︎ ↩︎ ↩︎
Written by

Tré LaRosa
Tré LaRosa is a consultant, scientist, and writer in the Washington, DC area with extensive experience working in research (basic, translational, and clinical) and on patient-reported outcomes. He has also written extensively on neuroscience, pulmonology, and respiratory conditions, including from the patient perspective. He enjoys learning, reading, writing, spending time outdoors, and telling everybody about his mini golden retriever, Duncan.