Pediatric spirometry: Strategies for success

According to the Asthma and Allergy Foundation of America, about 4.6 million children have asthma, making it the leading chronic disease among children under 18 years old.1 Despite its prevalence, asthma is not easy to diagnose in children simply because it often presents as the usual seasonal cold or allergy.2 When a child has a persistent cough, wheezing, and shortness of breath, parents want a precise diagnosis with access to the appropriate medications and care plan. Aside from collecting a family medical history and performing a thorough physical exam, a lung function test with spirometry is crucial.
While spirometry is non-invasive and cost-effective, it is often underutilized in assessing and diagnosing children, primarily due to the inherent challenges of obtaining accurate results in this age group.3 However, a skilled and trained healthcare provider who can effectively guide and engage a child with the correct technique should be able to collect optimal results even from children as young as four years old.3 In fact, a 2001 study published in the American Journal of Respiratory and Critical Care Medicine found that most 6-year-old children could perform reproducible spirometry within 15 minutes with proper direction.4
Although mastering the specific spirometry testing techniques for pediatrics may require practice, the potential benefits of obtaining an accurate diagnosis make the effort worthwhile.
Pediatric spirometry tips for providers #
Initial interventions #
Achieving optimal results begins before the patient is even in the office. Ensure all equipment works correctly and that enough supplies, such as mouthpieces and nose clips, are available to avoid distractions once the patient arrives. If applicable, review a recent history and physical, previous pulmonary function test results, and obtain an accurate height and weight before testing.
The following tips will help obtain quality spirometry results.
Preparing for the test #
Creating a comfortable environment is key to a successful spirometry test. If the patient seems anxious, spend extra time explaining the test and showing them the equipment that will be used. This approach can help alleviate their anxiety and improve their cooperation during the test.
Demonstrate the proper placement of the mouthpiece and how to create a tight seal. Explain that the tongue should stay under the mouthpiece rather than inside, as it can block air while breathing in or out.
Describe how they will take a few normal breaths in and out, then a huge breath in, and then blow out rapidly for as long as possible. The analogy of blowing hard, like they are trying to blow out all the candles on a gigantic birthday cake, helps with motivation. Give them a chance to practice before the test begins.
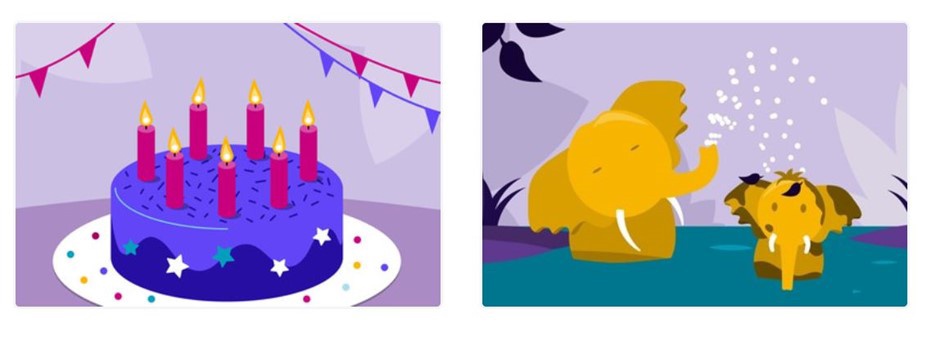
Examples of interactive pediatric incentives, available with EasyOne Connect software, that help to encourage pediatric patients to achieve maximum spirometry results.
Positioning #
Give the option to sit or stand for the test, as either position will produce an accurate result. If the patient chooses to sit, have them sit straight and note their position for future testing.
Coaching, encouragement, and visual incentives #
Enthusiastic, animated coaching, encouragement, and effective visual incentives are crucial for getting the best test results.
EasyOne Connect software provides simple, effective visual testing incentives for pediatric patients, including a birthday cake incentive and an elephant incentive (see above). These incentives can help the patient quickly understand the breathing maneuvers and can help make it more of a game than a “test,” reducing stress and increasing engagement.
Provide robust verbal encouragement as the patient watches the visual prompts. For example, once the patient is ready, encourage them to, “Take a deep breath and BLOW, BLOW, BLOW” until the test is complete.
After each attempt, positive feedback is crucial. Letting the patient know the results were good and asking if they think they can do an even better job on the next try can boost their confidence and encourage them to perform better in subsequent attempts. This approach is particularly effective with older pediatric patients who have tested before, as they often appreciate their success and are eager to improve on the next attempt.
Challenges and rewards #
Although there are specific challenges with pediatric pulmonary function testing, providing proper guidance and motivation for pediatric patients can usually lead to obtaining high-quality spirometry test results. Young patients require a child-friendly environment, age-appropriate instruction, and adequate time to understand proper maneuvers to obtain accurate results.5
There is little doubt that spirometry remains a relatively simple and objective test. It continues as an irreplaceable assessment tool for healthcare providers to make clear diagnoses, guide medication management, and influence ongoing care for pediatric patients.6
Asthma Facts. Asthma & Allergy Foundation of America. Accessed April 25, 2024. https://aafa.org/asthma/asthma-facts/ ↩︎
The role of pulmonary function testing in pediatrics. ndd Medical Technologies. Accessed April 25, 2024. https://nddmed.com/pulmonary-function-test-solutions/the-role-of-pulmonary-function-testing-in-pediatrics ↩︎
Burrill A, McArdle C, Davies B. Lung function in children: a simple guide to performing and interpreting spirometry. Paediatr Child Health. 2021;31(7):276-283. doi:10.1016/j.paed.2021.04.003 ↩︎ ↩︎
Eigen H, Bieler H, Grant D, Christoph K, Terrill D, Heilman DK, Ambrosia’s WT, Tepoer RS, Spirometric pulmonary function in healthy preschool children. Am J Respir Crit Care Med. 2001 Mar; 163(3 P1):619-23.
Doi.10.1164/ajrccm.163.3.2002054 ↩︎Lee E, Song JH, Chung EH, et al. Influence of Age on Effort Required to Complete Spirometry in Children and Adolescents. Allergy Asthma Immunol Res. 2022;14(6):752. doi:10.4168/aair.2022.14.6.752 ↩︎
Boonjindasup W, Marchant JM, McElrea MS, Yerkovich ST, Masters IB, Chang AB. Does routine spirometry impact on clinical decisions and patient-related outcome measures of children seen in respiratory clinics: an open-label randomised controlled trial. BMJ Open Respir Res. 2023;10(1):e001402. doi:10.1136/bmjresp-2022-001402 ↩︎
Written by

Allison DeMajistre
BSN, RN, CCRN
Allison DeMajistre is a freelance medical writer with a decade of clinical experience as a critical care registered nurse. She writes about cardiology, pulmonology, and several other medical topics. She strives to simplify complex medical information for patients and to write insightful and informative articles for health care professionals.