The financial impact of COPD on healthcare systems

Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory illness that affects approximately 480 million people1 and is the third leading cause of death worldwide.2 According to one study, COPD cases are on course to increase by 112 million in the coming years, resulting in an estimated 592 million individuals affected throughout the world by 2050.1
Besides its massive health burden, COPD poses significant economic implications, with long-term medication management, repeated hospitalizations, and outpatient medical management driving up costs for healthcare systems, communities, and individuals.
Early detection and diagnosis can help prevent morbidity, mortality, and the increasing financial pressure in countries around the world.3 Lung function testing is the standard for accurate COPD diagnosis. The results can help prompt early intervention and management to prevent excessive health-related costs and improve patient outcomes.
The cost of COPD #
The economic burden of COPD is multifaceted and involves both direct and indirect costs4 that combined are estimated to be $36 billion annually.5 Direct costs substantially impact healthcare systems and patients and generally involve exacerbation treatments, including hospitalizations, follow-up care, primary care visits, medications, laboratory testing, and rehabilitation costs. A 2024 study in CHEST Journal concluded that the total direct costs for COPD in the United States in 2019 were $31.3 billion and projected to grow to $60.5 billion in 2029.6 In Europe in 2020, the direct costs were estimated at 71 billion and projected to reach the trillions in 2050.7
However, the burden of COPD cannot be measured by direct costs alone. Although they are not as easily measured, indirect costs affect patients, their families, and their communities. Lost wages of the individual and family caregivers, employer-borne costs such as absenteeism and sick leave, disability, and impaired work performance all add to the immense and growing burden of COPD. Additionally, individuals face substantial out-of-pocket costs as exacerbations increase and hospitalizations become more frequent.7
Researchers continue to advocate for education and increased awareness of the long-term implications of COPD. Still, ultimately, the solution to easing the cost of COPD seems rooted in screening and early diagnosis.7
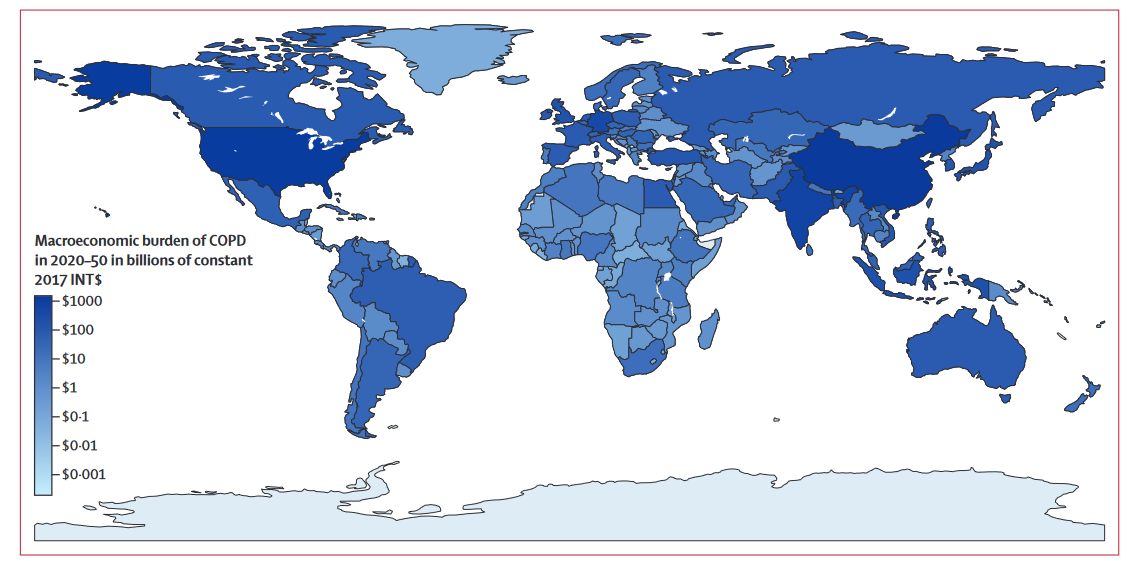
Macroeconomic burden of COPD in 2020–50 in billions of constant 2017 INT$. The darker a country’s color as displayed on the map, the higher its economic burden of COPD in billions of constant 2017 INT$. Grey areas represent countries within sufficient data. Photo source: https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(23)00217-6.pdf
Early detection with pulmonary function testing #
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) report focuses on providing strategies for diagnosing, treating, and managing COPD in the primary care setting.5
Clinical history and physical symptoms that warrant screening, such as a history of smoking or environmental exposure and presenting symptoms of productive cough and shortness of breath on exertion, can help lead clinicians in the right direction. Once initial screening is complete, spirometry is the first-line tool for effective diagnosis.
COPD diagnosis #
Spirometry measurements are essential to diagnose and determine COPD severity. It is also helpful in tracking response to treatment, medication adjustments, and monitoring the progression of the disease. Spirometry measures forced vital capacity (FVC), the maximal volume of air that can be forcibly exhaled after taking in the deepest possible breath, and forced expiratory volume in one second (FEV1), the maximal volume of air exhaled in the first second during an FVC maneuver. Clinicians can administer a short-acting bronchodilator and measure FVC and FEV1 after 10-15 minutes. Airflow limitation is confirmed if the FEV1 to FVC ratio is less than 0.70.5
Unfortunately, even though spirometry is required to confirm the diagnosis of COPD, it is not regularly utilized by primary care clinicians. According to one study, underuse is attributed to the uncertainty that spirometry is beneficial to the diagnosis of COPD, lack of resources, unfamiliarity with administering the test, and difficulty interpreting the results.5 Clinicians can benefit from hands-on training with meaningful feedback to gain confidence in performing spirometry in the primary care setting.8
Reducing the burden #
According to a 2015 article in Allergy and Asthma Proceedings, COPD resulted in 15.4 million doctor visits, 1.5 million emergency room visits, and 726,000 hospitalizations yearly.9 Limiting exacerbations and recognizing the severity of progressing disease is essential in limiting the overwhelming numbers. Unfortunately, COPD remains underdiagnosed by primary care physicians and has resulted in the notable health and economic burden facing healthcare and communities today.10
Early testing with spirometry can lead to accurate diagnosis and timely therapy initiation, which can often lead to better patient outcomes. It may also help alleviate the growing financial burden of COPD by substantially reducing direct and indirect costs for patients, communities, and healthcare systems.7
Easy and accessible spirometry testing #
Primary care providers don’t need to put off in-office spirometry any longer. The EasyOne spirometers are designed to be user-friendly and straightforward, reducing the need for a highly trained technician to be present for spirometry testing. Instead, virtually any healthcare professional can be trained quickly and easily on the EasyOne spirometry solutions.
Primary care providers and clinicians can position themselves to provide early and prompt diagnosis for at-risk patients that can begin easing the health and economic burden COPD has put on patients, communities, and healthcare systems for so long.
Global Burden of Chronic Obstructive Pulmonary Disease Through 2050 | Global Health | JAMA Network Open | JAMA Network. Accessed July 20, 2024. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2812622 ↩︎ ↩︎
The Global Economic Burden of chronic obstructive … Available at: https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(23)00217-6.pdf (Accessed: 26 August 2024). ↩︎
Number of COPD patients by 2050 predicted to hit nearly 600M. Accessed July 20, 2024. https://copdnewstoday.com/news/number-copd-patients-2050-predicted-hit-nearly-600m-globally/ ↩︎
Løkke A, Lange P, Lykkegaard J, et al. Economic Burden of COPD by Disease Severity – A Nationwide Cohort Study in Denmark. Int J Chron Obstruct Pulmon Dis. 2021;16:603-613. doi:10.2147/COPD.S295388 ↩︎
Yawn BP, Mintz ML, Doherty DE. GOLD in Practice: Chronic Obstructive Pulmonary Disease Treatment and Management in the Primary Care Setting. Int J Chron Obstruct Pulmon Dis. 2021;16:289-299. doi:10.2147/COPD.S222664 ↩︎ ↩︎ ↩︎ ↩︎
Mannino DM, Roberts MH, Mapel DW, et al. National and Local Direct Medical Cost Burden of COPD in the United States From 2016 to 2019 and Projections Through 2029. CHEST. 2024;165(5):1093-1106. doi:10.1016/j.chest.2023.11.040 ↩︎
Agarwal D. COPD generates substantial cost for health systems. Lancet Glob Health. 2023;11(8):e1138-e1139. doi:10.1016/S2214-109X(23)00304-2 ↩︎ ↩︎ ↩︎ ↩︎
Office Spirometry in Primary Care for the Diagnosis and Management of COPD: National Lung Health Education Program Update | Respiratory Care. Accessed July 20, 2024. https://rc.rcjournal.com/content/63/2/242/tab-pdf ↩︎
May SM, Li JTC. Burden of chronic obstructive pulmonary disease: Healthcare costs and beyond. Allergy Asthma Proc. 2015;36(1):4-10. doi:10.2500/aap.2015.36.3812 ↩︎
The Quality of Care and Economic Burden of COPD in the United States: Considerations for Managing Patients and Improving Outcomes. Accessed July 20, 2024. https://www.ahdbonline.com/articles/3223-the-quality-of-care-and-economic-burden-of-copd-in-the-united-states-considerations-for-managing-patients-and-improving-outcomes ↩︎
Written by

Allison DeMajistre
BSN, RN, CCRN
Allison DeMajistre is a freelance medical writer with a decade of clinical experience as a critical care registered nurse. She writes about cardiology, pulmonology, and several other medical topics. She strives to simplify complex medical information for patients and to write insightful and informative articles for health care professionals.