A simple guide to COPD
COPD is a chronic, progressive lung disease characterized by airflow limitation, commonly caused by smoking, air pollution, or genetic factors. It leads to breathlessness, chronic cough, wheezing, and reduced activity, often worsening over time through exacerbations and comorbid conditions such as heart disease and asthma. With over 250 million people affected worldwide and many cases remaining undiagnosed, early detection using spirometry is crucial for accurate diagnosis, effective management, and reducing the disease’s global health burden.

COPD is a common respiratory disease affecting people worldwide. Chronic cough, wheezing, and other symptoms make breathing more difficult and worsen quality of life. Causes of COPD include smoking, air pollution, and genetics. COPD is often accompanied by different diseases, including asthma and heart disease, so spirometry testing is critical for proper diagnosis.
This guide will discuss COPD’s definition, symptoms, prevalence, causes, diagnosis, and comorbidities. Understanding COPD and recognizing its symptoms is crucial to receiving appropriate treatment and lessening COPD’s burden.
COPD definition and symptoms #
According to Iheanacho et al, COPD “is characterized by incurable, progressive airflow restriction and has various clinical forms, including emphysema and chronic bronchitis.”1 The Global Initiative for COPD (GOLD) explains that when harmful gases and particles enter the airways and lungs, an inflammatory response occurs.2 GOLD notes that while COPD is common, preventable, and treatable, it is chronic and progressive with exacerbations and concurrent diseases leading to a patient’s worsening condition.2
Common symptoms of COPD include: dyspnea, also known as shortness of breath, chest tightness, wheezing, and cough that may or may not include phlegm, otherwise known as sputum.3 Patients often experience fatigue and are limited in their activities.3 A patient’s symptoms may increase more severely over a period of time in what’s known as an exacerbation, thus requiring additional support.3
How common is COPD? #
More than 250 million people around the globe are affected by COPD.1 COPD consistently ranks as one of the top 10 leading causes of death worldwide, but its position moves based on the country and year.4 Looking at 2022 U.S. age-adjusted mortality rates, data show chronic lower respiratory diseases as the sixth leading cause of death in the United States.4 Taking a more expansive view, WHO’s Global Health Estimates show that COPD was the third leading cause of death worldwide in 2019.5 It dropped to the fourth spot in 2021 due to the emergence of COVID-19.5
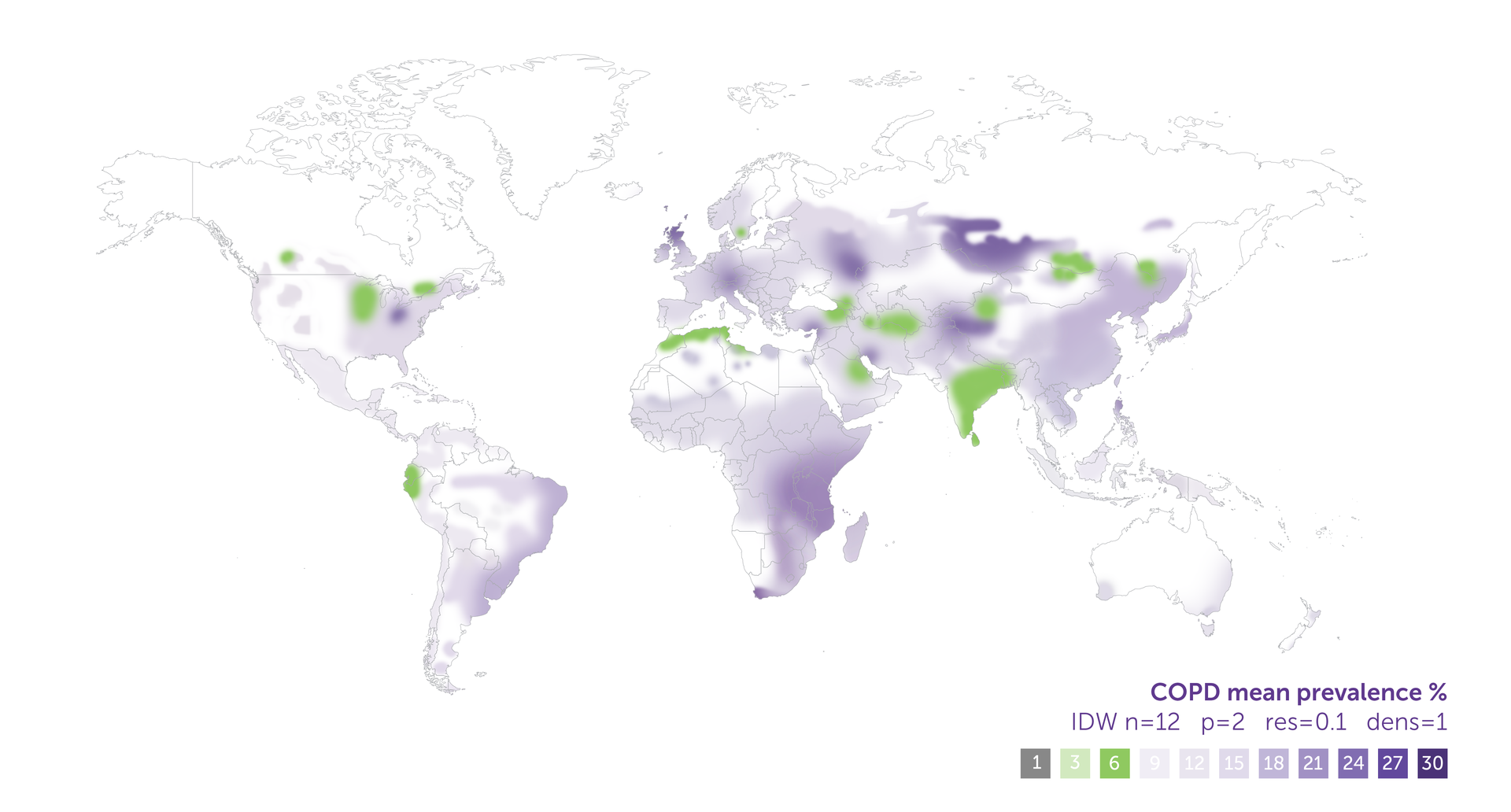
Geographic distribution of COPD prevalence displayed by ERS Geographic Information System Maps.
Despite these high numbers, many people live with COPD without knowing it. Shockingly, global estimates of those who are undiagnosed reach upwards to 95 percent.6 Undiagnosed COPD cases lead to a heavier physical, emotional, and financial burden on individuals and society. So, what can be attributed to misdiagnosis and underdiagnosis of COPD? Studies show that spirometry, a type of lung function test that diagnoses COPD, is underutilized in some parts of the world for several reasons, including the cost of some devices, limited resources, and contradictory information.6 Misconceptions about the causes of COPD may also lead to confusion. While there is a high prevalence of COPD among smokers, non-smokers can develop it, too.
What causes COPD? #
While a variety of factors cause COPD, around 90 percent of cases are attributed to smoking.7 Smoke’s chemicals are so damaging to the airways and lungs that even those exposed to secondhand smoke may be at greater risk of COPD.7
Air pollution is another major contributor to COPD. In fact, it is the leading cause among those who have never smoked.8 When harmful particles and gases enter the lungs due to outdoor, indoor, or occupational air pollution, those with COPD are at greater risk of exacerbations, hospitalization, and even death.8
Genetics can also play a role. Most people have alpha-1 antitrypsin to protect their lungs7, but some have a deficiency caused by SERPINA1 gene mutations8 that exposes their lungs to harm. This is called alpha-1 antitrypsin deficiency or AATD.3 While this is not the only genetic variant connected with greater COPD risk, it is the most pertinent compared to the small effect sizes of other variants.8
How is COPD tested? #
Spirometry, a type of lung function test, is primarily used to diagnose COPD.9 The test involves a patient breathing into a mouthpiece attached to the spirometer, while the spirometry device records various parameters. These measurements are then compared to established reference values to assess lung function and identify any abnormalities. At-risk patients experiencing symptoms will particularly benefit from spirometry to aid in diagnosis and management of symptoms.10 Additional tests include peak expiratory flow test, arterial blood gas test, chest X-ray, and CT scan.9
EasyOne spirometry machines - tailored solutions for every practice.
Explore our spirometry machines
What comorbidities accompany COPD? #
COPD is often accompanied by other conditions in which are known as comorbidities. Heart conditions are one type of comorbidity for good reason.11 The heart and lungs make up a close system within the body.11 When airflow is limited, such as with COPD, the heart is forced to work even harder.11 Research across years of study shows that a cardiovascular disease diagnosis is more likely for COPD patients.12 Hypertension occurs more frequently, and the risk of heart failure and cardiac dysrhythmia, among others, is a whopping two to five times greater.12 Consequently, patients with heart conditions benefit from lung testing.
Asthma is another comorbidity. This is known as Asthma-COPD Overlap Syndrome (ACOS). ACOS leads to worse outcomes with more frequent exacerbations, a faster lung function decline, and a greater chance of death, so it’s essential to differentiate the two to ensure proper treatment.2 However, shared symptoms can create confusion. In addition to tests, questionnaires, a patient review, and an examination, a careful comparison of features is needed.2
Conclusion #
You, as a provider, play a crucial role in COPD diagnosis. By incorporating spirometry into your practice, you can identify COPD sooner, thus helping patients receive the care they need before the disease progresses. Early intervention can impact patient outcomes, improved quality of life, and reduced healthcare burdens and costs. Make spirometry a routine part of your practice today, and be the difference your patients need.
Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic burden of Chronic Obstructive Pulmonary Disease (COPD): A systematic literature review. International Journal of Chronic Obstructive Pulmonary Disease [Internet]. 2020 Feb 26 [cited 2025 March 28]; 15:439 60. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7049777/. doi: 10.2147/COPD.S234942 ↩︎ ↩︎
Diagnosis of Diseases of Chronic Airflow Limitation: Asthma, COPD and Asthma-COPD Overlap Syndrome (ACOS) [Internet]. Global Initiative for Asthma; 2014 [cited 2025 Mar 28]. Available from: https://ginasthma.org/wp-content/uploads/2019/11/GINA_GOLD_ACOS_2014-wms.pdf ↩︎ ↩︎ ↩︎ ↩︎
Patel N. An update on COPD prevention, diagnosis, and management: The 2024 GOLD Report. The Nurse Pract. [Internet]. 2024 Jun [cited 2025 March 28];49(6):29-36. Available from: https://journals.lww.com/tnpj/fulltext/2024/06000/an_update_on_copd_prevention,_diagnosis,_and.6.aspx. Doi: 10.1097/01.NPR.0000000000000180 ↩︎ ↩︎ ↩︎ ↩︎
Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2022. U.S. Department of Health and Human Services; 2024 Mar [cited 2025 Mar 28]. Available from: https://www.cdc.gov/nchs/data/databriefs/db492.pdf ↩︎ ↩︎
The top 10 causes of death [Internet]. World Health Organization; 2024 Aug 7 [cited 2025 Mar 28]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death ↩︎ ↩︎
LaRosa T. Increased utilization of spirometry: The solution to both mis- and underdiagnosed lung conditions [Internet]. 2023 Mar 22 [cited 2025 Mar 28]. Available from: https://nddmed.com/blog/2023/increased-utilization-of-spirometry-the-solution-to-both-mis-and-underdiagnosed-lung-conditions-across-the-world/ ↩︎ ↩︎
Causes: Chronic Obstructive Pulmonary Disease (COPD) [Internet]. NHS; [updated 2023 Apr 11; cited 2025 Mar 28]. Available from: https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/causes/ ↩︎ ↩︎ ↩︎
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Pocket guide to COPD diagnosis, management, and prevention: A Guide for Health Care Professionals [Internet]. 2024 ed [cited 2025 Mar 28]. Global Initiative for Chronic Obstructive Lung Disease, Inc.; 2023, 2024. Available from: https://goldcopd.org/2024-gold-report/ ↩︎ ↩︎ ↩︎ ↩︎
Diagnosis [Internet]. U.S. Department of Health and Human Services; [updated 2024 Oct 4; cited 2025 Mar 28]. Available from: https://www.nhlbi.nih.gov/health/copd/diagnosis ↩︎ ↩︎
Haynes JM, Kaminsky DA, Ruppel GL. The role of pulmonary function testing in the diagnosis and management of COPD. Respiratory Care [Internet]. 2023 Jul 1 [cited 2025 Mar 28];68(7):889–913. Available from: https://www.liebertpub.com/doi/abs/10.4187/respcare.10757. doi:10.4187/respcare.10757 ↩︎
DeMajistre A. How do the heart and lungs work together? [Internet]. 2023 Aug 30 [cited 2025 Mar 28]. Available from: https://nddmed.com/blog/2023/heart-lungs-how-they-work-together/ ↩︎ ↩︎ ↩︎
Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. The Lancet Respiratory Medicine [Internet]. 2015 Aug [cited 2025 Mar 28]; 3(8):631–9. Available from: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(15)00241-6/abstract. doi:10.1016/s2213-2600(15)00241-6 ↩︎ ↩︎
Written by

Kelly Sicard
MA
Kelly M. Sicard is a freelance writer with an M.A. in English & Creative Writing who spent over a decade working for a non-profit lung health organization. She lives in New Hampshire with her husband, daughter, and black labrador and enjoys reading, writing, listening to stories, appreciating nature, and spending time with family.