A simple guide to reading spirometry test results – Tips from Buddy
Understanding spirometry test results is made easier with guidance from Buddy, who explains key lung function values, common testing errors, and best practices for accurate assessment. The guide emphasizes proper coaching, consistent patient effort, and avoiding mistakes such as incomplete exhalation, air leaks, or interrupted maneuvers to ensure reliable and reproducible results. With practical, step-by-step tips and clear explanations, Buddy empowers both clinicians and patients to interpret spirometry outcomes confidently and support effective respiratory care.
Hello! Buddy here again! Today we’re talking about reading spirometry test results. Spirometry, as you may know, is a powerful tool for diagnosing and monitoring respiratory conditions, especially asthma and chronic obstructive pulmonary disease (COPD).
Spirometry Basics #
Last time, we discussed the importance of good coaching in yielding accurate and reliable spirometry results. Spirometry can be challenging for patients. We want to ensure we get acceptable results the first time around. As a reminder, I can help with that — as a spirometry coach, I help to build rapport, provide clear instructions, demonstrate good form, and give encouragement so that patients can feel comfortable and give their best effort.
Now that we’ve covered a few tips for performing spirometry, let’s discuss some common spirometry terms.
- FEV1: Forced expiratory volume in the 1st second
- FVC: Forced vital capacity. This is the total amount of air exhaled during spirometry.
- FEV1/FVC Ratio: A key indicator of airway obstruction. Usually represented as a decimal.
- Percent (%) Predicted: A patient’s results compared to the reference values based on their height, age, ethnicity, and biological sex, expressed as a percentage.1
Spirometry Tips #
There are a few common errors that occur during spirometry. Let’s discuss those and how to resolve them.
To start, instruct the patient to begin spirometry with the biggest breath in possible to completely fill the lungs—this full inhalation is critical—followed by an explosive exhalation as hard and fast as they can.
Patients must not slow or abruptly stop airflow in the first few seconds of blowing air out. To address this, check patient’s posture and encourage the patient to keep blowing continuously until their lungs are completely empty and no more air is coming out—I, Buddy, can help let you and your patients know when you’ve reached the end!
To produce an acceptable spirometry maneuver, it’s important to ensure the test remains uninterrupted. This includes ensuring the patient doesn’t cough in the middle of the test. If this occurs — or to prevent it from occurring — encourage the patient to drink water.
Another important note when performing spirometry is to ensure there are no air leaks, as even small leaks could affect the accuracy of the results. Make sure to have the patient seal their lips tightly around the mouthpiece and use a nose clip to prevent air from escaping through their nose. This helps ensure that all the air blown out is measured correctly for the most accurate results.
Patients should perform at least three acceptable and reproducible trials to ensure that enough data is collected to sufficiently assess the patient.
EasyOne spirometry machines - tailored solutions for every practice.
Explore our spirometry machines
Abnormal Spirometry Results #
The main purpose of spirometry is to assess whether a patient is experiencing obstruction or restriction and to what degree
Obstructive pulmonary diseases, including COPD, asthma, and cystic fibrosis, are characterized by reduced airflow and decreased airway diameter, which can be due to inflammation, mucus plugging, or smooth muscle contraction (usually in asthma). This often shows up on spirometry as reduced FEV1/FVC ratio. The lower the number, the more significant the obstruction. This ratio is decreased usually (but not always) because the patient has a lower FEV1 than would be expected for their demographics.
Restrictive patterns, on the other hand, can be due to pulmonary fibrosis, pulmonary edema, heart failure, and obesity. Restrictive pulmonary diseases are rare and result in a decline in lung volume. On a spirometry test, this looks like reduced FVC and VC. Flow limitations (FEV1/FVC) are generally unaffected, and if anything, can be slightly elevated.
Step-by-Step Guide to Interpreting Spirometry Results #
Now that we’ve discussed some spirometry basics and results, let’s discuss interpreting the results. To do so, there are four steps, each of which will be described below:
Step 1: Check the quality of the test
Step 2: Assess FEV1 and FVC compared to normal lung function using z-score
Step 3: Check FEV1/FVC ratio
Step 4: Assess for reversibility if bronchodilator was used
Step 1: Check the quality of the spirometry test #
The quality of the test should be assessed according to American Thoracic Society (ATS) and European Respiratory Society (ERS) guidelines, shown below.2 In other words, was the spirometry performed in an acceptable and reproducible manner.
While an A or B grade is ideal for test acceptability and repeatability, physicians can still gather valuable insights from other grades, as long as they interpret the results with appropriate caution.
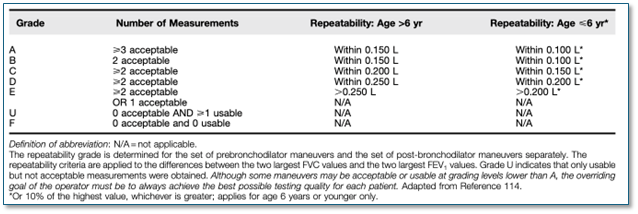
Figure 1: Grading System for FEV1 and FVC
Step 2: Assess FEV1 and FVC compared to normal lung function using z-score #
Once it’s determined whether the PFT (Pulmonary Function Test) quality is acceptable, it’s time to analyze the patient’s FEV1 and FVC values using z-score.
Prior to 2021, the patient’s FEV1 and FVC values were compared to percent predicted to assess severity of pulmonary disease. In 2021, ATS/ERS guidelines were updated to assess the patient’s pulmonary disease through z-score.3 These values are below. Z-scores enable a clinician to assess how far a patient’s observed function is from the normal population through standard deviations. This method has been found to be more consistent across age and sex than percent predicted.34
Z-score values for assessing severity of pulmonary disease:
- Mild: –1.65 to –2.5
- Moderate: –2.51 to –4.0
- Severe: <–4.
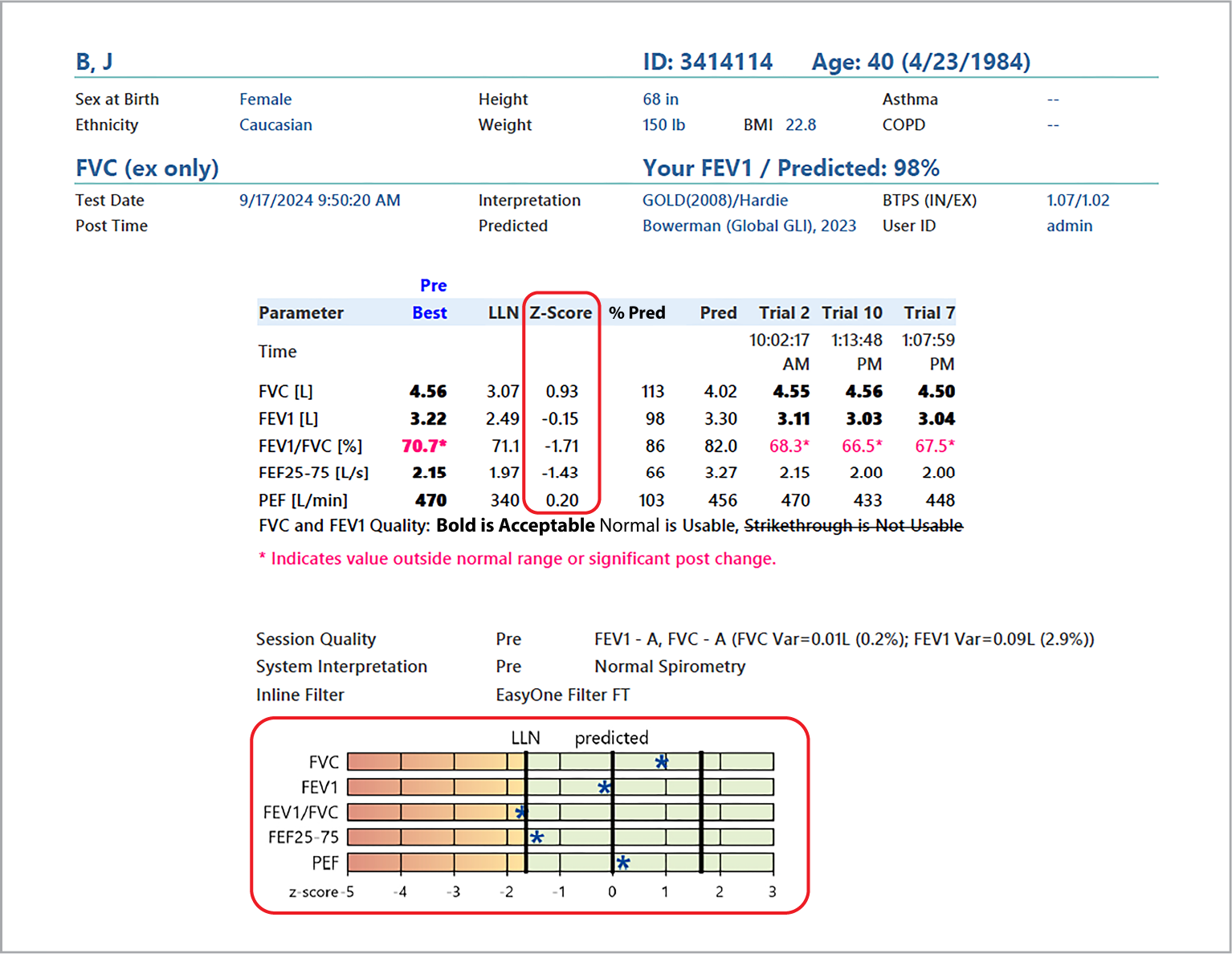
Step 3: Check FEV1/FVC ratio #
Once FEV1 and FVC predicted values are assessed, the FEV1/FVC ratio is the next part of the interpretation to discern obstruction or restriction or both.
Most of this has already been discussed above, but below is a handy guide for general traits for identifying obstruction or restriction. These cut-points are useful for interpretation, but the ATS/ERS guidelines emphasize that there is a degree of uncertainty involved.3
Normal lung function: FEV1 and FVC above 80% predicted; FEV1/FVC ratio above 0.7.
Obstructive lung disease: FEV1 below 80% predicted; FVC can be normal or reduced but usually to a lesser degree than FEV1; FEV1/FVC ratio below 0.7.
Restrictive lung disease: FEV1 is normal or mildly reduced; FVC below 80% predicted; FEV1/FVC ratio normal, so above 0.7.
Step 4: Assess for reversibility if a bronchodilator was used #
Since bronchodilators are often used to treat pulmonary conditions, it’s also helpful to evaluate the degree of which a bronchodilator reverses the decrease in pulmonary function. To that end, it’s recommended that a patient perform spirometry in the absence of their bronchodilator and then post-bronchodilator.
In the case of patients that do see an improvement in either or both their FEV1 and FVC with the use of bronchodilators, it’s important to emphasize that “reversibility” does not mean complete elimination of obstruction,2 but rather that airway obstruction may not be fixed.
In 2021, ATS/ERS released updated guidance defining what qualifies a positive bronchodilator response — a change of 10% or more of predicted value.3
Conclusion #
Spirometry is essential in managing pulmonary diseases, so it’s of the utmost importance to ensure patients succeed as best as they can in performing their pulmonary function tests. It’s also essential that the clinic administering the test understands how best to interpret the results.
Our newest product, the EasyOne Sky, aims to redefine this process with the help of me, Buddy!
If you would like to learn more, please take a few minutes to either submit a sales form for more information and a live demo, or please register for one of our live training events!
*Disclaimer The information provided in this guide is for informational purposes only and is not intended as medical advice. We are not medical professionals and do not offer diagnoses or treatment recommendations. This guide is meant to support understanding of spirometry test results and should not replace professional medical judgment.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). SPIROMETRY FOR HEALTH CARE PROVIDERS. 2017;7(1):4. ↩︎
Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70-e88. doi:10.1164/rccm.201908-1590ST ↩︎ ↩︎
Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1). doi:10.1183/13993003.01499-202 ↩︎ ↩︎ ↩︎ ↩︎
Miller MR, Cooper BG. Reduction in T LCO and survival in a clinical population. Eur Respir J. 2021;58(5):2002046. doi:10.1183/13993003.02046-2020 ↩︎