Diagnosing asthma in pediatrics: How good coaching leads to accurate spirometry results
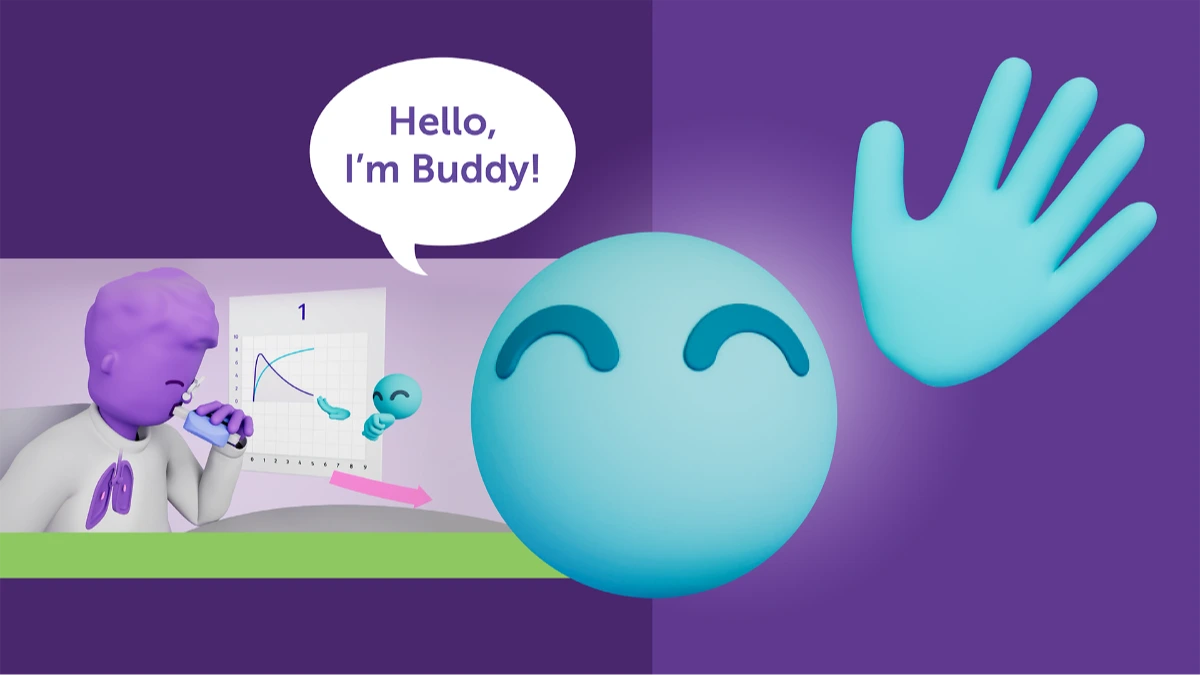
High-quality pediatric spirometry is essential for accurately diagnosing asthma in children, yet many young patients struggle to perform the test correctly. Effective coaching—using simple, kid-friendly explanations, visual demonstrations, and engaging digital tools like Buddy—helps children as young as four deliver reliable results. With proper guidance, clinicians can confidently assess airflow obstruction and bronchodilator response, making spirometry a powerful and dependable diagnostic tool in pediatric asthma care.

Asthma is the most common chronic disease in children, affecting millions worldwide. 1
Yet diagnosing it in kids—especially those under 12—can be tricky. Symptoms like wheezing, coughing, and shortness of breath often overlap with other conditions, and young patients may struggle to perform spirometry correctly. That’s why spirometry, paired with a skilled coach like Buddy, is a game-changer in pediatric asthma diagnosis and management.
Why Spirometry? #
Spirometry is recognized as the standard for assessing lung function. In children over age 4 it helps: 2
- Detect airflow obstruction
- Assess reversibility after bronchodilator use
- Monitor response to treatment over time
But here’s the catch: kids need guidance to perform the test properly. Without it, results can be misleading—or unusable.
EasyOne spirometry machines - tailored solutions for every practice.
Explore our spirometry machines
Coaching: The secret ingredient to pediatric spirometry #
Children don’t instinctively know how to take a deep breath and blow out forcefully for six seconds. That’s where coaching makes all the difference. A great spirometry coach should:
- Use kid-friendly language and analogies (like “blow out birthday candles”)
- Demonstrate the maneuver visually
- Offer enthusiastic encouragement and feedback
Making spirometry engaging with visual incentives #
At ndd, we’ve designed tools like Buddy, our new spirometry coach, and animated incentives (think elephants and birthday cakes!) to help kids stay focused and motivated. These tools:
- Turn testing into a game
- Provide real-time feedback
- Help children understand what’s expected
With the right support, even children as young as 4 or 5 can produce reliable spirometry results. 3
What clinicians look for in spirometry #
Once a high-quality test is completed, clinicians assess:
- FEV₁/FVC ratio: A reduced ratio may indicate obstruction
- Bronchodilator response: An increase in FEV₁ of ≥12% and ≥200 mL supports asthma diagnosis 4
These objective measures, combined with a child’s history and symptoms, may help confirm asthma or point to another condition.
Final thoughts on spirometry in pediatrics #
Diagnosing asthma in children requires more than just a stethoscope—it takes patience, creativity, and coaching. With the right approach, spirometry becomes not just possible, but powerful. And when kids feel supported and understood, they’re more likely to give their best effort.
Want to see how Buddy, our friendly spirometry coach, can help your practice? See Buddy in action here.
Global Asthma Network. The Global Asthma Report 2022. ↩︎
Global Initiative for Asthma (GINA). “Global Strategy for Asthma Management and Prevention.” 2023 update. ↩︎
Beydon et al., “An Official American Thoracic Society/European Respiratory Society Statement: Pulmonary Function Testing in Preschool Children,” American Journal of Respiratory and Critical Care Medicine, 2007. ↩︎
Global Initiative for Asthma [GINA], 2024 ↩︎