Beyond clinical value: Measuring revenue impact of spirometry

Value-based care is changing healthcare and encouraging integrated delivery networks (IDNs) and healthcare systems to think differently about how they deliver care their patients. This is particularly true for those with chronic pulmonary conditions such as chronic obstructive pulmonary disease (COPD).
Spirometry, which is a useful tool for the entire disease journey for people with chronic pulmonary conditions, is a small one-time investment with big upside for healthcare systems. Spirometry can thread the needle that systems must carefully account for: Spirometry, when leveraged effectively, can improve patient outcomes, reduce direct costs by reducing admissions and readmissions, and also serve as an efficient revenue generator. By implementing this essential pulmonary function test into outpatient and primary care offices, healthcare systems can reap significant long-term savings and revenue gains.
Spirometry drives revenue #
COPD, while common, is frequently under- and misdiagnosed.1 One of the primary reasons for this is due to lack of access to reliable and accurate spirometry, which is necessary to confirm a diagnosis. Further, spirometry is a crucial tool for adequate management of COPD. Accurate use of spirometry can prevent late diagnoses, which are associated with poorer clinical outcomes.1 Multiple studies and organizations, including the Global Initiative for Obstructive Lung Disease (GOLD) have recommended that increased usage of spirometry in those with symptoms, especially in primary care clinics, can help address the crisis of late diagnoses.
After the initial diagnosis, routine follow-up with spirometry is essential to help clinicians hone in on the right treatments and monitor disease progression.
Although spirometry remains underutilized, the availability of portable, reliable spirometry devices makes it easy to implement across multiple sites and office locations. As a result, spirometry can both improve patient outcomes and generate additional revenue.
Breaking down the return on investment on spirometry #
Let’s discuss the possible return-of-investment that clinics can get by instituting spirometry. Spirometry is a direct revenue generator in the form of reimbursement and billable testing, explained more below. But there are multiple ways that spirometry indirectly helps clinics’ bottom lines.
There is evidence that effective use of spirometry can improve outcomes in patients, potentially reduce readmissions, and reduce emergency room visits.2 3There’s an additional way spirometry can ameliorate budget constraints, that’s even more hidden and obscure, but no less important: Patients with more severe COPD tend to use more healthcare services, including being readmitted more often for reasons other than COPD.3 In other words, when COPD is diagnosed early and effectively managed with the assistance of spirometry, patients are admitted less often for comorbidities and other risk factors.
Billable spirometry codes #
There are several CPT codes clinics can use to apply for reimbursement in the US: 94010, 94014, 94016, 94060, 94200, 94375. Below is a table describing each of the codes that can be billed for spirometry and the estimated reimbursement, based on United States Medicare Average as of January 2026.
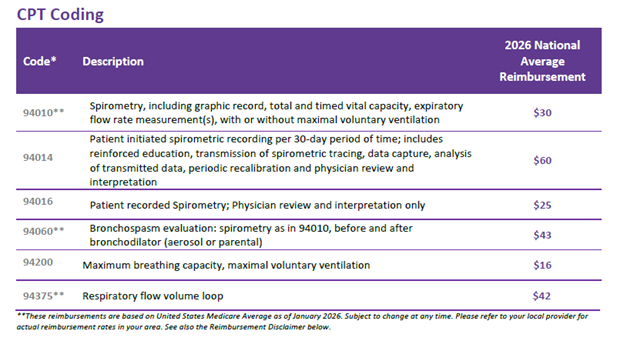
United States Medical Average - January 2026 - Spirometry CPT Codes
What’s the revenue opportunity? #
Direct revenue for spirometry is generated through reimbursement. Consider a 500-bed hospital performing 1,000 tests per year. At a reimbursement rate of $43 per test (using CPT code 94060), performing spirometry on the right patients can generate $43,000 a year in direct annual revenue! Assuming a spirometer costs approximately $2,000, that’s an ROI of 2,050%!
Curious about your potential revenue? Use our ROI calculator to find out how adding spirometry could positively impact your clinic's financial performance.
Calculate now!
Cost savings by reducing COPD readmissions #
Admissions alone are costly, but readmissions, which are quite common, are where costs really begin to accrue. Readmissions can lead to penalties based on the Hospital Readmissions Reduction Program (HRRP), and in general they are more costly. One study found that nearly one in five COPD patients were readmitted for any cause within 30 days.4 They were primary readmitted due to COPD exacerbation, sepsis, acute respiratory failure, pneumonia, and heart failure.4
According to the Agency for Healthcare Research and Quality (AHRQ), initial COPD admissions cost approximately $12,700 in 2020. When readmitted within 30 days for COPD, readmissions are even costlier than the initial admission. A Healthcare Cost and Utilization Project brief found that readmissions where COPD was the principal reason for readmission were 18% more expensive than initial admissions for COPD. Readmissions can also be considered preventable, pending specific criteria, which is why it can lead to penalties or reduced reimbursement.
One study sought to parse out how much of the total cost of COPD was driven by readmissions. The authors found that approximately 30% of all cost associated with COPD were due to readmissions.5 Though all readmissions, especially those that are unrelated to COPD, can’t be fully prevented, many can be and should be prioritized.
Conclusion #
Early diagnosis through spirometry is a key component of improving system-wide control of COPD and reducing the number of patients who go undiagnosed or undertreated. Spirometry can also be a worthwhile investment for delivery networks and healthcare systems to prioritize as a form of sustainable revenue generation in the form of reimbursement and as a cost-savings tool in the form of improving care management and thus reducing admissions, readmissions, and ER visits.
With the help of accessible, portable, economical, and reliable devices, such as ndd EasyOne spirometry devices, clinics can generate sustainable revenue while improving patient outcomes.
Discover the long-term financial potential of implementing spirometry by using our ROI calculator today!
Larsson K, Janson C, Ställberg B, et al. Impact of COPD diagnosis timing on clinical and economic outcomes: the ARCTIC observational cohort study. Int J Chron Obstruct Pulmon Dis. 2019;14:995-1008. doi:10.2147/COPD.S195382 ↩︎ ↩︎
Loh CH, Genese FA, Kannan KK, Lovings TM, Peters SP, Ohar JA. Spirometry in Hospitalized Patients with Acute Exacerbation of COPD Accurately Predicts Post Discharge Airflow Obstruction. Chronic Obstr Pulm Dis Miami Fla. 2018;5(2):124-133. doi:10.15326/jcopdf.5.2.2017.0169 ↩︎
Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic Burden of Chronic Obstructive Pulmonary Disease (COPD): A Systematic Literature Review. Int J Chron Obstruct Pulmon Dis. 2020;Volume 15:439-460. doi:10.2147/COPD.S234942 ↩︎ ↩︎
Khamooshi P, Shaka H, Velazquez G, Ovie O, Obiaigwe H, Mohamoud I. RATE AND REASONS FOR 30-DAY READMISSION FOLLOWING COPD: A UNITED STATES ANALYSIS. CHEST. 2021;160(4):A1899. doi:10.1016/j.chest.2021.07.1682 ↩︎ ↩︎
Press VG, Konetzka RT, White SR. Insights about the economic impact of chronic obstructive pulmonary disease readmissions post implementation of the hospital readmission reduction program. Curr Opin Pulm Med. 2018;24(2):138-146. doi:10.1097/MCP.0000000000000454 ↩︎
Written by

Tré LaRosa
Tré LaRosa is a consultant, scientist, and writer in the Washington, DC area with extensive experience working in research (basic, translational, and clinical) and on patient-reported outcomes. He has also written extensively on neuroscience, pulmonology, and respiratory conditions, including from the patient perspective. He enjoys learning, reading, writing, spending time outdoors, and telling everybody about his mini golden retriever, Duncan.