Best practices for pulmonary function testing in COVID-19

We’ve talked before about best practices for restarting pulmonary function testingprograms, but the recommendations that came from the ATS working group were heavily focused on traditional, in-hospital PFT labs. Arguably, that setting is still the top-dog in this arena, but the ongoing pandemic has shown us that top-box healthcare practices have to be ready to break out of traditional mindsets in order to provide optimal care. The explosive adoption of telehealth services has gotten the lion’s share of attention from those who track healthcare innovation, but pulmonary function testing offers an additional return on investment, without the uncertainty of regulatory changes or reimbursement questions. It may not be the sexiest or most obvious choice for an add-on service, but it’s a relatively simple way to add value to practices and healthcare systems, as well as monitor the health impacts of respiratory diseases (including COVID-19), thus protecting entire communities.
Expanding existing practices #
As we move into new phases in the pandemic, those big PFT labs mentioned above are indeed beginning to open back up. However, many seem to be taking a relatively conservative approach; indeed, this is the recommendation of that ATS working group. In order to protect patients and staff, robust screening programs, additional personal protective equipment requirements, and waiting-area protocols are being implemented. These help keep people safer, but they also tend to decrease throughput. Add that to the backlog of tests created by pandemic-related shutdowns, and wait times for tests are skyrocketing. Considering that it could be a heavy lift to get people into the PFT lab even before the COVID-19 era for a variety of reasons (after all, who wants another trip to the doctor’s office?), and access is quickly becoming an issue across the country.
The good news is that many ambulatory practices already have spirometry testing available. This is an excellent time to bring those dusty machines that have been sitting idle, consider upgrading them to newer, more accurate machines with lower maintenance requirements, train up a few staff members to ensure high quality and consistency, and start testing! Testing in the office setting offers a number of benefits to patients, perhaps most notably that they already have an existing relationship and degree of trust with you and your staff. Having that trust goes a long way to establishing the rapport necessary to get patients to respond to coaching and instruction and to perform at their peak. These are both essential components to high-quality test results, which means that you have a built-in advantage over a facility filled with strangers, regardless of their expertise. In addition, your office is likely more familiar than your local PFT lab, making it a comfortable environment. It might even be easier for patients to get to, again lowering the risk of losing patients to follow-up.
Of course, this does mean that practices will have to make some adjustments to their workflows, but many of these adjustments have likely already been made in response to the novel coronavirus anyway. Proper pre-screening procedures and scheduling protocols (as indicated by the status of the pandemic in your community) can help limit interactions with sick or potentially sick patients, and appropriate PPE and patient flow strategies can facilitate a safe experience for patients and staff alike. Successful programs can improve patient care and relieve the burden of established pulmonary testing resources all at once.
Expanding testing for COVID-19 and beyond #
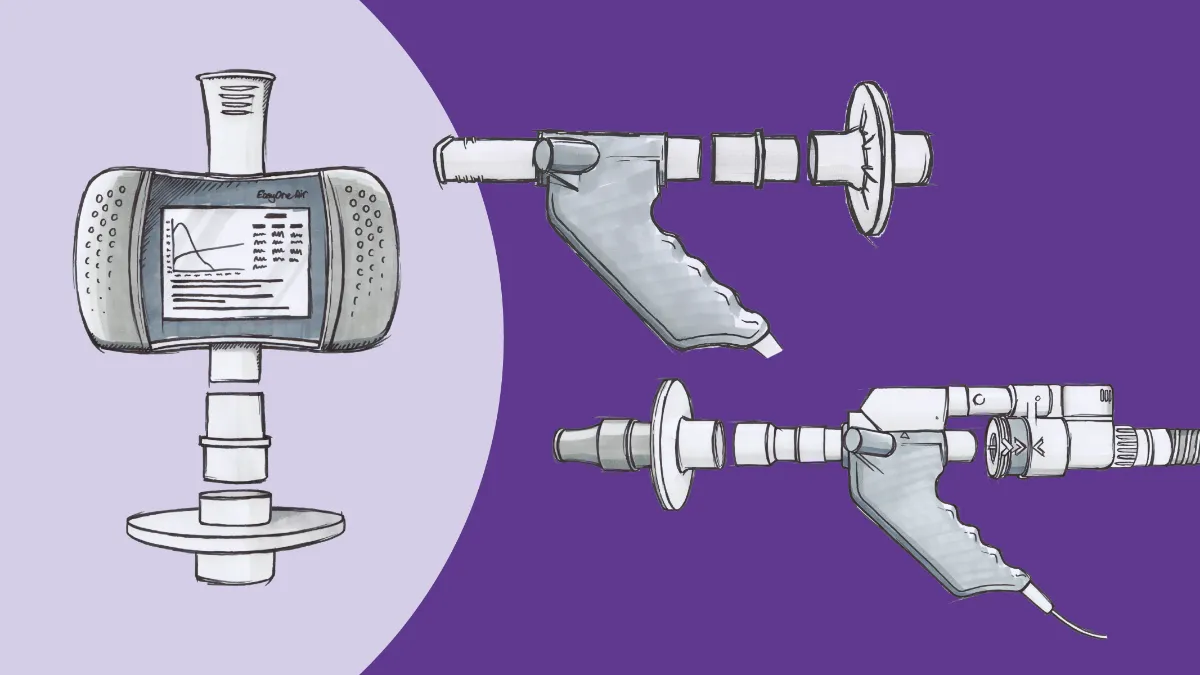
Many offices have not yet taken the plunge into setting up spirometry programs. However, just as it’s a great time to expand, it’s a great time to get in the game! Pulmonary function technology has really never been more accessible, financially, or operationally, than it is today. Based on national average reimbursement rates, a device like ndd’s EasyOne Air spirometer can pay for itself in as little as 40 tests, with only the relatively low cost of consumables going forward. This rapid return on investment makes spirometry testing programs economically feasible for virtually any practice, a key consideration after the financial impacts of the pandemic throughout the primary care world.
There are two paths a launch strategy can take. The first is to develop a process for routine testing of all post-COVID patients. While the last six months may seem like they’ve dragged on for six years, we have to keep things in perspective; we still have virtually no idea what the true long-term effects of this disease will be. We don’t know how it’s going to affect people with previously-healthy lungs, we don’t know how it’s going to affect those with COPD or asthma, and we don’t know how it’s going to affect those with pulmonary fibrosis or other interstitial conditions, because even those survivors designated “long-haulers” have had the disease less than a year. To be clear, this is in no way minimizing their plight, as this cohort appears to have significant quality of life impairment at this point. We simply don’t know how long it will last, or what we can do about it. So, in order to develop any kind of effective management strategy down the road, having longitudinal lung function data will be crucial.
Much still needs to be learned about what pulmonary function data will look like in the setting of COVID‑19, in the acute phase or after the fact. However, certain patterns are starting to come into focus. For example, topline data from a study done in China found relatively low prevalence of airflow dysfunction (either obstructive or restrictive patterns)1. However, looking a little more closely, a full 25% of the entire cohort was found to have decreased total lung capacity (TLC, a hallmark of restrictive lung disorders), and nearly half those having “severe” COVID-19 related pneumonia (defined in the study as having a respiratory rate greater than 30, severe respiratory distress, or an oxygen saturation of less than 93%) were found to have low TLC. It’s not always a straightforward process to pick out patients who may have low TLC by spirometry, but seeing a restrictive pattern on a spirogram can at least get clinicians thinking along those lines ( and there are some additional possibilities that we’ll discuss in a minute). Similar data, again suggesting a restrictive disorder than can be red-flagged by spirometry, were found in another Chinese study2, and a third (albeit rather small) Italian study was again consistent with these findings3.
There are some major caveats to these studies. First and foremost, these three studies represent the current body of knowledge on pulmonary function testing in the setting of COVID-19 searchable on PubMed. The studies are also quite small, with a grand total of 180 subjects between all three of them, with the vast majority of them (110) coming from a single study. We can make some preliminary inferences, especially as our understanding of how the SARS-CoV-2 virus itself works, but we still have a long way to go to truly understanding the impacts of a “post-COVID syndrome.” However, that does speak to the urgency of making the full range of pulmonary function testing, including spirometry, available as widely as possible.
The second strategy is to take a more measured approach, and develop a traditional spirometry program focusing on patients with an active respiratory complaint. Even before the pandemic, access to spirometry was limited in the primary care world, with 25 to 50% of providers (depending on type and location) reporting they did not have access to spirometer in their office4. These providers would either proceed to diagnose empirically (increasing their risk of misdiagnosis and suboptimal clinical decision making) or refer their patients to a PFT lab (increasing the burden on the patient and risking them failing to follow up). We’ve already covered how the pandemic has obviously worsened the latter issue, but empirical diagnosis may well continue to grow riskier. Consider this: We know that even people who have asymptomatic cases of COVID-19 are at risk for cardiac complications5. We also know that SARS-CoV-2 not only damages cardiac tissue, it also has an affinity for airway epithelial cells.6 It therefore is reasonable to presume that at least some asymptomatic cases will have delayed-onset pulmonary effects, and that these people will eventually seek care for dyspnea. The best way to differentiate between obstructive conditions like asthma or COPD and restrictive ones like pulmonary fibrosis (a leading contender for post-COVID lung problems) is through pulmonary function testing, and that can start in primary care.
Regardless of the approach, increased spirometry testing also has a significant add-on benefit for anyone with respiratory disease: It can open the door to pulmonary rehabilitation. Pulmonary rehab is a chronically-underutilized therapy for a wide range of breathing problems, spanning both the restrictive and obstructive domains. However, most insurance carriers (including Medicare) require documentation of impaired spirometry before they will even consider paying for a program. Thus, by not ensuring that every potential patient has a test, clinicians are leaving one of the most potent tools we have behind in the toolbox.7
Not just spirometry #
We’ve focused a great deal on spirometry so far because that has traditionally been the most familiar and accessible pulmonary function tests in the ambulatory care world. But now is a good time to point out that not all the change in the world these days is for the worse, and technology has made major strides in the past decade. These days, full-featured pulmonary function testing equipment is within reach of any practice, without the need for physically remodeling your clinic space or massive capital investment. This modern equipment can serve as a “lab in a box,” bringing advanced tests like diffusion transfer capacity (DLCO) and lung volumes analysis to the clinic floor, reducing the burden on patients (and care coordinators) even more.
As wonderful and useful as spirometers are, these full-PFT machines may end up being even more valuable in the post-COVID. Recall that relatively few patients ended up with significant defects in their airflow mechanics; however, that doesn’t mean they escaped without any injury. In the largest study, a full 47% of COVID-19 patients had decreased diffusion capacity for carbon monoxide (DLCO, also sometimes known as transfer capacity) and, just as with the spirometric values, the risk for worsening DLCO increased with disease severity. Again, this aligns with our growing understanding of COVID-19 as not just a pulmonary condition, but a cardiovascular one. It also may explain why there have been so many reports of the so-called “happy hypoxics,” who have acute COVID-19 with remarkably low oxygen saturation readings, but no significant dyspnea (at least, until their system can’t handle it anymore and they crash).8
The availability of this technology opens up many new possibilities across the continuum of care. Much like spirometry, research applications appear to be the ‘low-hanging fruit’ here, especially as we work to improve our care for COVID long-haulers and understand any potential long-term effects. We may also see a point-of-care diagnostic role for this equipment, in properly-outfitted clinics and emergency departments; patients with other symptoms or possible exposures can be rapidly assessed for DLCO defects and triaged appropriately. Wider adoption of this technology would have positive effects even outside of COVID-19 as well, considering DLCO has been suggested as a more accurate prognostic indicator than traditional airflow obstruction9. These machines are also able to measure lung volumes, helping to confirm the presence of restrictive lung disorders in COVID-19 survivors and having prognostic utility in other chronic lung conditions, such as cystic fibrosis10. Just imagine what applications will continue to be found, as these devices become more commonplace.
It’s become cliché at this point to say that we still don’t know what the new normal of healthcare will look like. We’ve been through a lot over the last six months or so, and it’s true that there’s been a lot of disruption, a lot of uncertainty, and a lot of negativity as we contemplate the idea that nothing will ever be the same. However, every one of the challenges that we have faced this year also represents an opportunity to do better for those in our care. It may seem counterintuitive, and it’s certainly easier said than done, but now is the time to think big, to ride the wave of disruption in order to reshape healthcare. We’re starting to see how the forced implementation of telehealth has had a positive impact; imagine what easy access to pulmonary function testing could do. What would faster access to results do for your practice? What would it do for patient satisfaction? Care coordination? Research?
The future doesn’t have to be something to fear. You just need to be as prepared as possible to face it. With this kind of pandemic, and with chronic respiratory conditions already on the rise, that means figuring out the right pulmonary testing solution for your practice and ensuring you’re able to make the best clinical decisions, so your respiratory patients don’t have to waste a single breath.
Mo X, Jian W, Su Z, et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;55(6). doi:10.1183/13993003.01217-2020 ↩︎
Huang Y, Tan C, Wu J, et al. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir Res. 2020;21(1):163. doi:10.1186/s12931-020-01429-6 ↩︎
Fumagalli A, Misuraca C, Bianchi A, et al. Pulmonary function in patients surviving to COVID-19 pneumonia. Infection. 2020. doi:10.1007/s15010-020-01474-9 ↩︎
COPD: Tracking Perceptions of Physicians Who Diagnose and Treat COPD (2017) | National Heart, Lung, and Blood Institute (NHLBI).; 2017. https://www.nhlbi.nih.gov/health-topics/all-publications-and-resources/copd-tracking-perceptions-physicians-who-diagnose-and. Accessed December 11, 2018. ↩︎
Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. doi:10.1001/jamacardio.2020.3557 ↩︎
Ehre C. SARS-CoV-2 Infection of Airway Cells. N Engl J Med. 2020;383(10):969-969. doi:10.1056/NEJMicm2023328 ↩︎
Celli B. Pulmonary rehabilitation. In: Post T, ed. UpToDate. Waltham, MA; 2020. https://www.uptodate.com/contents/pulmonary-rehabilitation. Accessed September 16, 2020. ↩︎
Dhont S, Derom E, Van Braeckel E, Depuydt P, Lambrecht BN. The pathophysiology of “happy” hypoxemia in COVID-19. Respir Res. 2020;21(1):198. doi:10.1186/s12931-020-01462-5 ↩︎
Balasubramanian A, Kolb TM, Damico RL, Hassoun PM, McCormack MC, Mathai SC. Diffusing Capacity Is an Independent Predictor of Outcomes in Pulmonary Hypertension Associated With COPD. In: Chest. Vol 158. Elsevier Inc; 2020:722-734. doi:10.1016/j.chest.2020.02.047 ↩︎
O’Neill K, Tunney MM, Johnston E, et al. Lung Clearance Index in Adults and Children With Cystic Fibrosis. Chest. 2016;150(6):1323-1332. doi:10.1016/j.chest.2016.06.029 ↩︎