DLCO: A simple guide
Spirometry is probably the most well-known of the pulmonary function tests. Even people who don’t remember they’ve had a ‘PFT’ will remember the test where someone yelled at them to, “keep blowing, keep blowing!” However, there is another test that can provide a wealth of information on how the lungs are actually exchanging the gases that keep us alive, shedding additional light this on critical lung function. That test is known as the diffusion capacity of lung for carbon monoxide, or DLCO.
More than good air in, bad air out #
Recall basic lung physiology, where oxygen enters the alveoli, works its way across the alveolar membrane, and enters the bloodstream to join up with the hemoglobin molecules that transport it throughout the body. Once it reaches a particular destination, oxygen serves as a sort of cellular fuel, powering the chemical reactions that provide energy to our metabolism. Carbon dioxide is given off as a waste product of this reaction, and it takes oxygen’s place in circulation as the ‘spent’ blood travels back to the lungs for a refresh.
This is, of course, a rather simplified version of the actual processes, and that is especially true with the alveolar membrane part. You see, moving from an area of high concentration to an area of low concentration (the chemical definition of diffusion) is only one piece of the gas transport equation. There are a variety of factors that can affect how easily oxygen and carbon dioxide move across that tiny partition. For example, low hemoglobin levels provide fewer sites for oxygen to bond with, reducing overall oxygen intake. Physical thickening of the barrier, as seen in interstitial lung diseases, also makes it more difficult to move molecules through. Lower overall alveolar surface area, as in emphysema, also provides lower opportunity for gas exchange. The list goes on, but, measuring the rate at which the molecules are moving can give keen insight into how the lungs themselves are operating.
DLCO testing #
Testing DLCO is straightforward, as well. The fastest and most common procedure, known as the single-breath technique, starts with the test subject breathes through a PFT mouthpiece for a few breaths to get used to the setup (and don’t forget the nose clips for this one). The technologist then tells them to breath out fully, all the way to their residual volume (the amount of gas that remains in the lungs to keep the alveoli open). While the subject exhales, the technologist engages the system, sealing the circuit and priming the test gas cylinder. As soon as the subject begins to inhale again, the system delivers the test gas, which is specially formulated with trace amounts of carbon monoxide (as well as oxygen and some inert gases). The subject is coached to inhale sharply and fully, all the way to their total lung capacity. For many, the next phase is the most difficult, as the subject now has to hold their breath for a full 10 seconds to allow a measurable amount of gas to exchange. After the breath hold, the subject can exhale naturally, all the way back to their residual volume, flushing out any remaining carbon monoxide from their lungs.
Why is such a gas used for the test? Well, it turns out that carbon monoxide has a much greater affinity for hemoglobin than oxygen does; hundreds of times greater, in fact. This, combined with the fact that carbon monoxide uptake in the lungs is less affected by cardiac output than oxygen would be, allows for rapid calculation of DLCO. Measurement is done by discarding the first 25% or so of the exhaled gas (which represents dead space ventilation only), comparing the carbon monoxide concentration of the next liter or so of exhalate, and then discarding the final volume of gas (which has had a significantly longer amount of time to transfer). As with other PFT data, the DLCO reading is compared to predicted values based on patient factors, which yields the final result.
Use in PFT diagnostic #
These measurements are often underrated when it comes to diagnosis and patient assessment. For example, while FEV1 from spirometry is often cited as an indicator of severity and predictor of mortality in COPD, DLCO has actually been demonstrated to be the most powerful predictor of survival in people with COPD.1 It has also been advanced as a potential tool to predict hospitalizations for COPD exacerbations.2 DLCO measurements have long been established as early-warning signs of things like interstitial lung disease (even before airflow indicators), and can also help distinguish between interstitial lung diseases and mechanical issues like chest wall defects.3
Preliminary studies have also suggested DLCO may be a powerful tool in the monitoring of COVID-19. Those people enduring post-COVID-19 syndrome (often called ‘long COVID’) have often been found to have lower DLCO readings, which makes sense considering many long COVID symptoms, such as brain fog and fatigue, are also associated with lower oxygen levels.4 Tracking DLCO readings in these patients may eventually give us a better understanding of the cause of long COVID, as well as point us in the direction of better treatments.
Leveling up your PFT services #
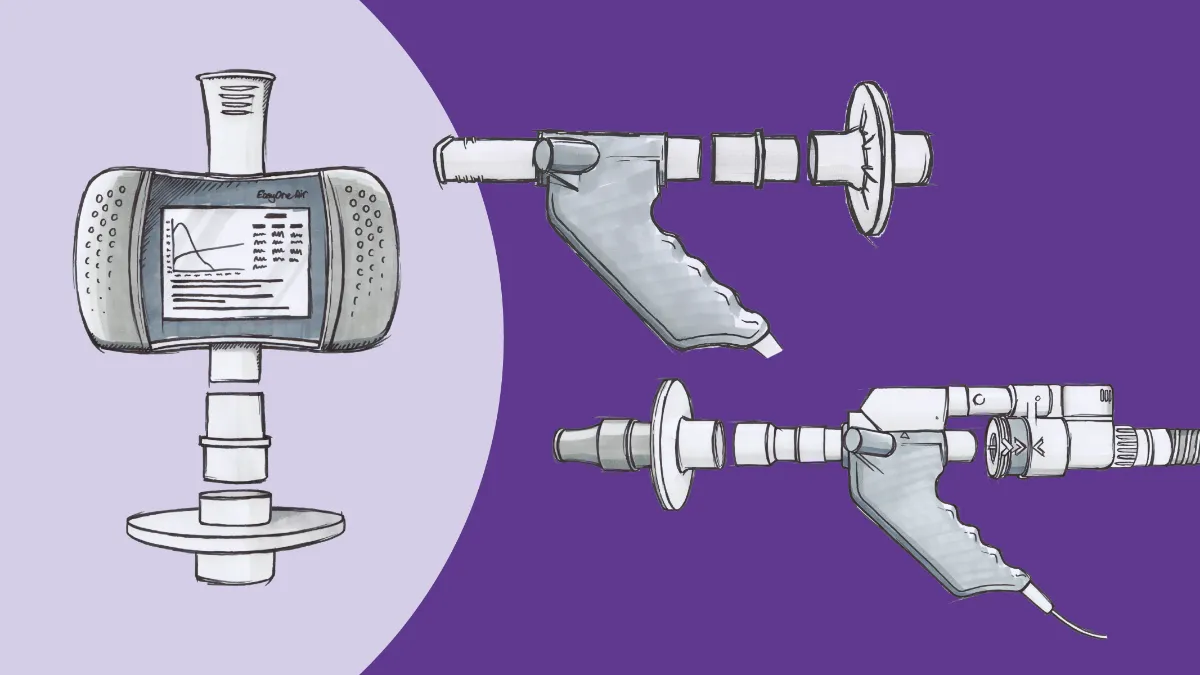
DLCO testing is a proven asset in patient assessment, but has flown under the radar because it has often been regarded as solely the purview of established pulmonary function laboratories. However, advancements in technology have made DLCO testing equipment much more accessible in a variety of practice environments, including primary care. Considering both the value it adds to patient care, the low impact on workflows and the added revenue stream PFT services provide, it’s almost a no-brainer to add DLCO testing to your list of services.
Balasubramanian A, Kolb TM, Damico RL, Hassoun PM, McCormack MC, Mathai SC. Diffusing Capacity Is an Independent Predictor of Outcomes in Pulmonary Hypertension Associated With COPD. In: Chest. Vol 158. Elsevier Inc; 2020:722-734. doi:10.1016/j.chest.2020.02.047 ↩︎
Balasubramanian A, Gearhart A, Fawzy A, et al. TP041 DIAGNOSIS AND RISK ASSESSMENT IN COPD / Thematic Poster Session Diffusing Capacity Is a Predictor of Hospitalizations Among Patients with Airflow Obstruction Receiving Care in an Academic Health System. www.atsjournals.org. Accessed October 27, 2021. ↩︎
Enright P. Office-based DLCO tests help pulmonologists to make important clinical decisions. Respir Investig. 2016;54(5):305-311. doi:10.1016/j.resinv.2016.03.006 ↩︎
Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, et al. Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis. Pulmonology. 2021;27(4):328-337. doi:10.1016/j.pulmoe.2020.10.013 ↩︎