DLCO: An old pulmonary function test with new promise

One of the major additions to the Global Initiative for Obstructive Lung Disease (GOLD) Guidelines in 2022 was the inclusion of guidance for the diffusing capacity of the lungs for carbon monoxide (DLCO), also known as transfer capacity of the lungs for carbon monoxide. Discovered when researchers learned that oxygen passively diffuses through the lung,1 DLCO, sometimes known as “a window on the pulmonary microcirculation,”2 is a complex pulmonary function test that evaluates the ability of a person’s lungs to transfer gas from inhaled air to the bloodstream.
In practice, DLCO is a simple to perform test, whereby the patient first fully exhales before inhaling the test gas — comprised of a very low percentage of carbon monoxide, oxygen, a tracer gas such as helium or methane, and nitrogen —3 then holding it in their lungs for 10 seconds. After this time has elapsed, the patient is asked to fully exhale. The exhaled gas is then analyzed to determine the concentration of the exhaled carbon monoxide and tracer gas giving clinicians a better understanding of a patient’s body’s ability to transfer oxygen from the air to their bloodstream and of the lung size.
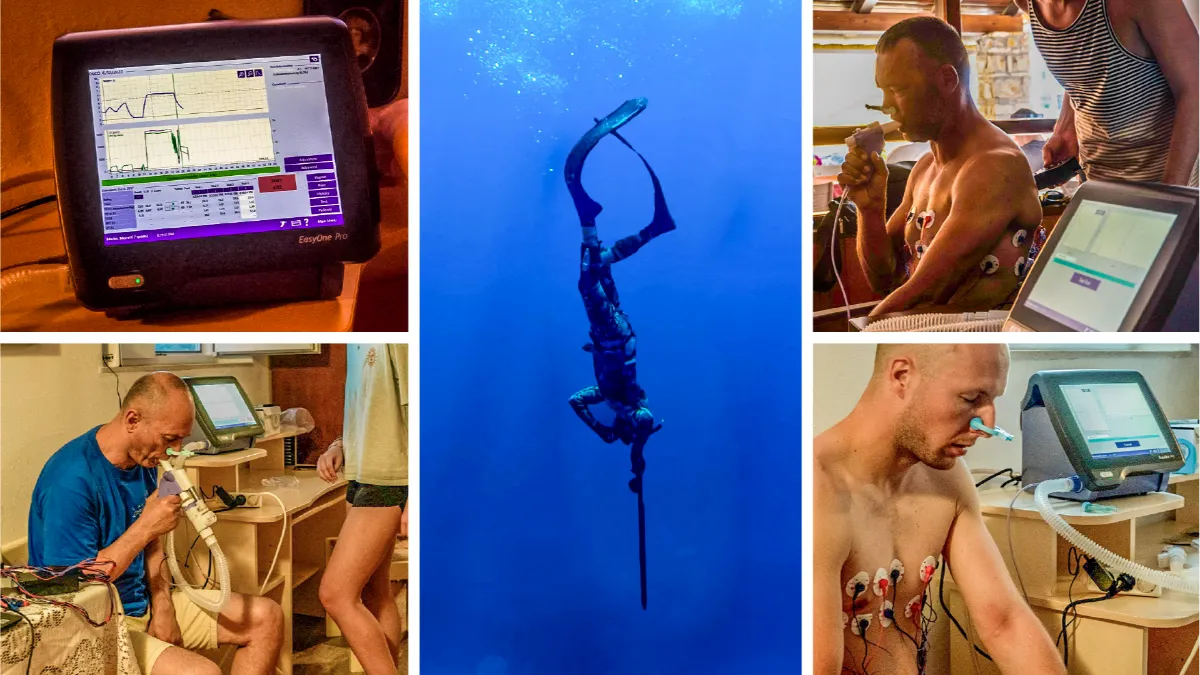
This test is over one hundred years old, so why has it only just recently been added to the GOLD Guidelines? It takes time, occasionally decades, for the medical and research community to understand something in great enough detail for it to become a part of clinical practice. Even when a test has promising evidence justifying its use, sometimes its non-use may be due to accessibility or systemic barriers such as price. Additionally, the DLCO test is a measurement of gas transfer, which itself is a nuanced topic. Despite these considerations, the DLCO test has now been added to the GOLD standard due to its many known benefits, the ease of the test, accessibility of instruments such as EasyOne Pro LAB and EasyOne Pro, and the contemporary understanding of the importance of measuring gas transfer.
The benefits of DLCO #
DLCO is the most powerful predictor of survival in patients with COPD #
In a study published by the European Respiratory Journal, DLCO was found to be not only one of the few variables “independently associated with survival,” but also the strongest prognostic indicator, whereas GOLD stage was not found to be as strongly predictive.4 The authors also concluded that their data, alongside other emerging evidence, suggests that death in COPD is associated to impaired vital capacity rather than airflow obstruction.4 DLCO has clinical use but its research use shouldn’t be dismissed: Understanding that COPD is associated with impaired vital capacity rather than airflow obstruction informs the field on COPD’s associated pathology.
DLCO is used as an indicator of lung disease severity #
Similarly to its ability to predict survival, DLCO is also a helpful indicator of lung disease severity. Lung disease exists on a continuum, not as a binary between perfectly healthy lungs and death. DLCO, in its predictive capacity, can be used to inform how severe somebody’s lung disease has already become.
DLCO can show a comorbidity of COPD in heart failure in patients #
Heart failure and COPD are frequent comorbidities due to cigarette smoking being a risk factor for both.5 DLCO measures the ability of somebody’s lungs to transfer oxygen to their bloodstream, so lung indices including DLCO can play a pivotal, even prognostic, role in conditions such as heart failure. 5In one review article published in the European Journal of Heart Failure, the authors recommended the use of both spirometry and DLCO in the initial work-up and the follow-up care of patients with heart failure.5
DLCO can assess the exacerbation and hospitalization risk in a COPD patient #
Again underscoring the various ways in which DLCO can be used to better characterize a patient with COPD, DLCO can be used to assess the likelihood of exacerbation 6and hospitalization risk in patients. In a study published in the journal Chest specifically investigating the implications of DLCO, the authors concluded “impairment in DLCO was associated with increased COPD symptoms, reduced exercise performance, and severe exacerbation risk,” and importantly, they emphasized this evidence was true “even after accounting for spirometry and CT evidence of emphysema.”6 All in all, DLCO is a strong indicator of a lot of morbidities associated with COPD.
DLCO is helpful in detecting drug-induced lung disease #
DLCO offers more sensitivity compared to spirometry in drug-inducedinterstitial lung disease, preceding changes in forced vital capacity 7and symptomatic deteriorating, offering a point where interventions can begin prior to the patient beginning to worsen.
Precision DLCO testing with EasyOne Pro
Discover the benefits
Additional benefits of DLCO monitoring #
- DLCO could be a helpful tool for monitoring COVID-19, as more than half of ICU-treated COVID-19 patients demonstrated impaired DLCO at four months follow-up.8
- DLCO can be used to inform differential diagnoses between COPD and asthma.9
- In a study published in the journal Chest, Balasubramanian et al demonstrated that DLCO is a “good prognostic tool” for unusually severe pulmonary hypertension.10
- In a 2016 study published in Chest comparing DLCO to CT-determined emphysema, de-Torres et al found that DLCO was useful in identifying which patients with COPD were at increased risk of lung cancer death.11
Conclusions #
DLCO clearly offers clinicians and researchers a major opportunity to better understand, characterize, diagnose, monitor, and predict the outcomes of patients with COPD, asthma, and other lung conditions. Though it’s an old test, its utility has become clear in recent years, as demonstrated by its inclusion in the GOLD standard. Fortunately, with the advent of portable tools such as the EasyOne Pro and EasyOnePro LAB, DLCO should become even more commonplace and widespread.
Chaouat A, Adir Y. Diffusing Capacity for Carbon Monoxide Is a Reflection of the Pulmonary Microcirculation, but Not Only. CHEST. 2020;158(2):455-457. doi:10.1016/j.chest.2020.03.033 ↩︎
DeCato TW, Hegewald MJ. Diffusing Capacity, the Too Often Ignored Lung Function Test in COPD. Chest. 2021;160(2):389-390. doi:10.1016/j.chest.2021.05.005 ↩︎
Executive Summary: 2017 ERS/ATS standards for single-breath carbon monoxide uptake€in€the lung
Brian L. Graham
https://www.thoracic.org/statements/resources/pft/DLCO-exec-summary.pdf ↩︎Boutou AK, Shrikrishna D, Tanner RJ, et al. Lung function indices for predicting mortality in COPD. Eur Respir J. 2013;42(3):616-625. doi:10.1183/09031936.00146012 ↩︎ ↩︎
What can we learn from pulmonary function testing in heart failure? - Magnussen - 2017 - European Journal of Heart Failure - Wiley Online Library. Accessed April 7, 2023. https://onlinelibrary.wiley.com/doi/full/10.1002/ejhf.946 ↩︎ ↩︎ ↩︎
Balasubramanian A, MacIntyre NR, Henderson RJ, et al. Diffusing Capacity of Carbon Monoxide in Assessment of COPD. Chest. 2019;156(6):1111-1119. doi:10.1016/j.chest.2019.06.035 ↩︎ ↩︎
Skeoch S, Weatherley N, Swift AJ, et al. Drug-Induced Interstitial Lung Disease: A Systematic Review. J Clin Med. 2018;7(10):356. doi:10.3390/jcm7100356 ↩︎
E E, R F, Öi E, et al. Impaired diffusing capacity for carbon monoxide is common in critically ill Covid-19 patients at four months post-discharge. Respir Med. 2021;182:106394. doi:10.1016/j.rmed.2021.106394 ↩︎
Neder JA, Berton DC, Muller PT, O’Donnell DE. Incorporating Lung Diffusing Capacity for Carbon Monoxide in Clinical Decision Making in Chest Medicine. Clin Chest Med. 2019;40(2):285-305. doi:10.1016/j.ccm.2019.02.005 ↩︎
Balasubramanian A, Kolb TM, Damico RL, Hassoun PM, McCormack MC, Mathai SC. Diffusing Capacity Is an Independent Predictor of Outcomes in Pulmonary Hypertension Associated With COPD. Chest. 2020;158(2):722-734. doi:10.1016/j.chest.2020.02.047 ↩︎
de-Torres JP, Marín JM, Casanova C, et al. Identification of COPD Patients at High Risk for Lung Cancer Mortality Using the COPD-LUCSS-DLCO. Chest. 2016;149(4):936-942. doi:10.1378/chest.15-1868 ↩︎
Written by

Tré LaRosa
Tré LaRosa is a consultant, scientist, and writer in the Washington, DC area with extensive experience working in research (basic, translational, and clinical) and on patient-reported outcomes. He has also written extensively on neuroscience, pulmonology, and respiratory conditions, including from the patient perspective. He enjoys learning, reading, writing, spending time outdoors, and telling everybody about his mini golden retriever, Duncan.