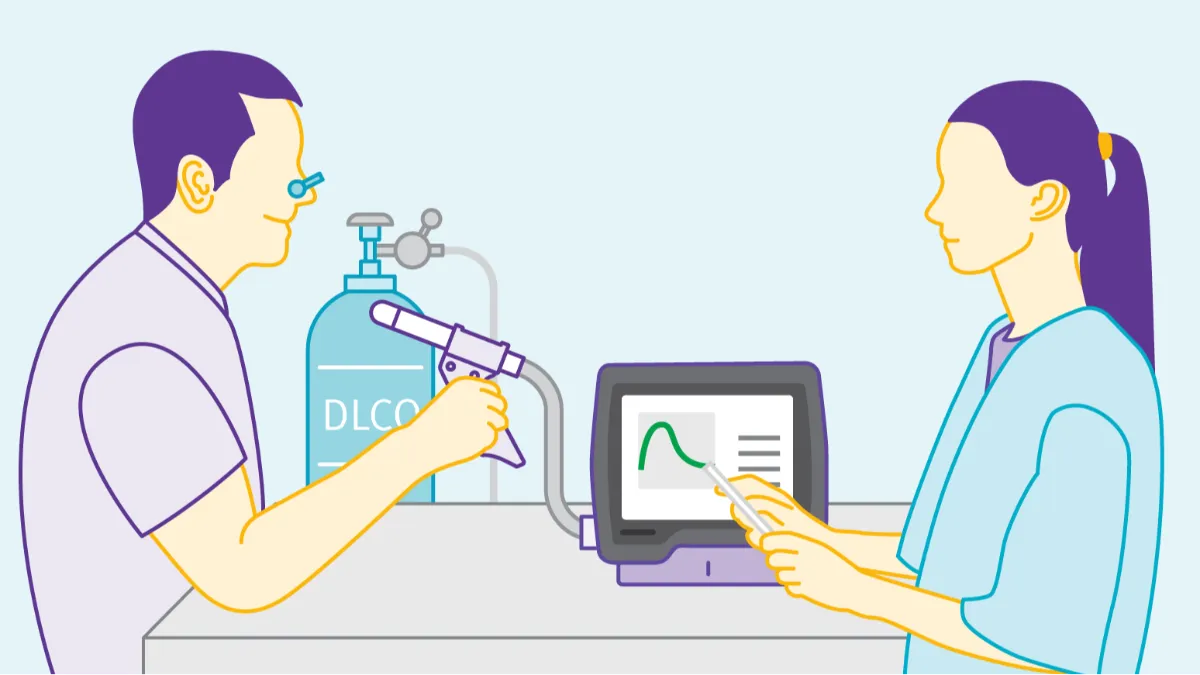
How to series: How to perform a DLCO test
While spirometry holds the crown as the most well-known pulmonary function test (PFT), evaluating how well oxygen and carbon dioxide transfer from the alveoli is also extremely useful in refining a diagnosis. This evaluation uses a test known as Diffusion Capacity of the Lung for Carbon Monoxide, occasionally also known as the transfer factor or simply DLCO. Historically, DLCO testing has been the domain of specialized laboratories equipped with intricate, complex devices, requiring patients to make yet another trip. However, modern PFT equipment has brought these tests out of the lab and to the point of care, enabling practices of virtually any scope to provide this important diagnostic service. In addition, PFT services at the point of care can provide an additional revenue stream and makes your practice truly patient centered.
DLCO indications #
Many of your patients would likely benefit from adding DLCO test results to their medical record. As useful and informative as spirometry is, it has certain limitations. For example, DLCO testing can help differentiate the damage caused by emphysema from issues brought on by obstructive bronchitis or undertreated/refractory asthma, allowing patients to be screened earlier for treatments like lung volume reduction procedures. It can help differentiate actual interstitial lung disease from poor patient effort, which can easily mimic the presence of a restrictive lung disease. It can even reveal uncommon conditions (or at least those thought to be uncommon due to otherwise low-quality testing) like pulmonary vascular disease and pulmonary hypertension.1 It is invaluable for prognostic and monitoring purposes in interstitial lung disease, and is simply under-utilized in a variety of respiratory disease states. That means significant missed opportunities for earlier diagnosis, better disease progression monitoring, and even research into mortality and quality of life measures. That, in turn, allows practices integrating DLCO testing into their routines to cover a great many gaps in knowledge and care across the healthcare continuum.
Ensuring DLCO testing success #
Now that your practice has decided to develop a DLCO testing program, there are a few things to consider before teeing up your first patient. In addition, there are some factors to keep in mind as you perform ongoing testing; while tests like DLCO are now relatively easy to perform, there are still certain tasks to perform in order to provide the highest quality test performance.
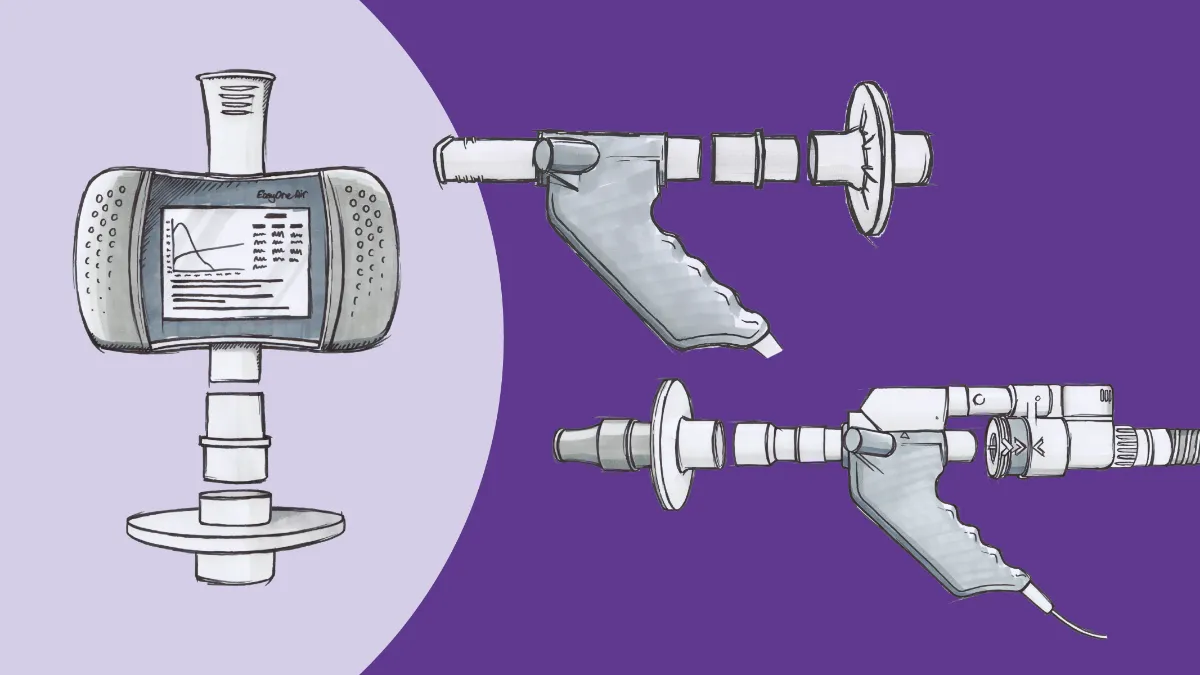
Equipment: Obviously, you need to make sure your equipment is up to the task. In most cases, that means time-consuming daily calibration checks and other routine maintenance. However, with the EasyOne Pro line, you can be confident in your results right from the start. The patented TrueCheck™ technology that these devices are built upon verifies the on-board gas analyzer with a five-point validation and linearization test. In addition, the TrueFlow™ technology that powers the entire ndd PFT product line, ensures accurate flow and volume detection through ultrasonic measurement. Occasional verification using a biological ‘control’ (for example, a healthy clinic employee) is still considered best practice, but the reliability of testing values given by ndd equipment has been clinically validated and peer-reviewed.2
A special consideration for DLCO testing is the precise gas mix used in testing. Carbon monoxide (CO) is used because it has an affinity for hemoglobin roughly 200 times greater than oxygen. A mere 0.3% of the test gas mixture is composed of CO. An additional 10% of the mixture is helium, which allows for the measurement of alveolar volume, an important consideration in the setting of emphysema. There is also roughly ‘room air’ levels of oxygen (generally 18-25%) to ensure safety, with the remainder of the gas composed of inert nitrogen. The gas must be obtained from a qualified medical gas dealer, to ensure all proportions are accurate to within 10% of their claimed volumes.
Patient: All relevant patient data should be entered prior to testing, especially as a valid spirometry testmust precede any DLCO measurement. This is because in order to know how much CO enters the bloodstream, the system has to know how much was inhaled into the lungs. Thus, the vital capacity must be measured, and the patient must be able to inhale to at least 90% of that vital capacity during the DLCO test. If available, a recent (or current, depending on equipment availability) hemoglobin level should be obtained and entered.
As with any other testing, it’s imperative to go over the test with the patient before moving forward. Explanations and demonstrations can go a long way into ensuring cooperation and good technique, both critical to getting the best possible data. The patient should also be comfortable, sitting upright, and able to hold the mouthpiece in their mouth, form a tight seal with the lips, and be able to tolerate nose clips. Water should be made available to assist with potential dry mouth between test attempts, and all infection control guidelines (including the use of filters, if applicable) should be maintained. Finally, it is important to keep the mouthpiece away from the patient at all times until ready to test, to ensure not even a trace of the test gas makes its way into the respiratory system, potentially contaminating results.
DLCO testing, testing #
Now it’s time to test. Much like with spirometry, proper execution of the testing maneuver is essential to reliable data. The DLCO technique is not necessarily as complicated as spirometry, but it can be difficult for patients to perform in its own way, depending on the respiratory status of the patient. It can be broken down into the following steps:
- Tidal breathing: Once the mouthpiece is inserted and the nose clips are in place, have the patient breath normally. This gives the patient a chance to get used to the equipment, and the clinician a chance to ensure the equipment is positioned properly and no leaks are detectible.
- Maximal exhalation: Once the patient is comfortable and ready, have them exhale comfortably (unforced) as much as possible, down to their residual volume (RV). In those patients with obstructive conditions, this may take an extended period. Standard recommendations call for this phase to take no longer than 12 seconds, in order to accommodate those with obstruction and enable them to get reasonably close to RV while not causing discomfort. Again, this facilitates inhalation to vital capacity and accurate gas volume measurement.
- Activation: While the patient is exhaling, the technician should start the test. This allows the system to ready itself to deliver the gas and seal the circuit. As soon as the end of exhalation is detected, the machine’s motor and valve unit close automatically and the mouthpiece is connected to the test gas source.
- Rapid, complete inhalation: The patient now takes a sharp maximal inhalation to their total lung capacity (TLC). The test gas is delivered through the entire breath, making it critical the patient gets as close to their previously measured vital capacity as possible. As mentioned, values of 90% of previous or greater are optimal, although value of 85% are acceptable if the measured alveolar volume during that test are also within 5% or 200 milliliters of the highest measured alveolar volumes of all attempted tests.
- Breath hold: The hardest part of the maneuver for many patients. Best practice calls for a 10-second breath hold, although there is some margin for error, which allows for an 8-12 second hold. This allows the CO gas to cross the respiratory membrane and bind with hemoglobin. It may be helpful to count the patient down, so they know exactly how much time is left in the hold. Other patients prefer to not have to think about it, so be sure to check individual preferences.
- Unforced exhalation: After time runs out, have the patient exhale without hesitation back down as low as they can go. The maneuver should last somewhere between 3-5 seconds (again, people with obstruction may take longer). The first 25% of the exhaled gas is discarded, as this represents deadspace ventilation that would create an artificially low reading. The next 50% of the gas sample is analyzed as the ‘true’ measurement of DLCO, and the last 25% is similarly discarded as it represents the gas with the longest time to transfer across.
- Relaxed inhalation: This helps signal the end of the test and allows the patient some time to recover.
End of the line #
Assuming the test went well and there are no data quality issues, those seven steps make up one successful effort. Additional research is needed to reveal what the ideal number of tests is to ensure repeatability and confirm reliability, but we do know more is not necessarily better. Performing five maneuvers can result in an increase in baseline carboxyhemoglobin (hemoglobin with carbon monoxide attached instead of oxygen) of 3-4%, which means the DLCO measurement will be decreased by a proportional amount.3 However, given that a single maneuver may also not be completely trustworthy due to a variety of human factors, that may not be sufficient for clinical decision making either. Thus, best practice recommendations suggest two maneuvers, separated by at least four minutes to allow for natural washout of the CO contained in the trace gas.4
On your own #
It is worth remembering that carbon monoxide never simply ‘diffuses’ across the respiratory membrane as we commonly think of the process. A variety of factors, including hemoglobin levels, alveolar surface area, even blood flow through the pulmonary capillaries can affect what is more properly called transfer of CO. Thus, it is imperative to account for these factors during the interpretation of DLCO results.
Chandra S, Shah SJ, Thenappan T, Archer SL, Rich S, Gomberg-Maitland M. Carbon monoxide diffusing capacity and mortality in pulmonary arterial hypertension. J Hear Lung Transplant. 2010;29(2):181-187. doi:10.1016/j.healun.2009.07.005 ↩︎
Gochicoa-Rangel L, Pérez-Padilla R, Vázquez-García JC, et al. Long-term stability of a portable carbon monoxide single-breath diffusing capacity instrument. Respir Care. 2017;62(2):231-235. doi:10.4187/respcare.04983 ↩︎
Zavorsky GS. The rise in carboxyhemoglobin from repeated pulmonary diffusing capacity tests. Respir Physiol Neurobiol. 2013;186(1):103-108. doi:10.1016/j.resp.2013.01.001 ↩︎
Graham BL, Brusasco V, Burgos F, et al. Executive summary: 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017;49(1). doi:10.1183/13993003.E0016-2016 ↩︎