September is Pulmonary Fibrosis Awareness Month
September means a lot of things to a lot of people. It’s time for back-to-school shopping, the football season kicks off, and certainly everyone looks forward to International Talk Like a Pirate Day every September 19th. September is also Pulmonary Fibrosis Awareness Month, an opportunity to bring attention and advocacy to a chronic respiratory condition that affects hundreds of thousands of people around the world. As the calendar flips over from late summer to early autumn, let’s take a closer look at this often-overlooked disease state.
Pulmonary Fibrosis Basics #
Pulmonary fibrosis (PF) is not merely a single disease, but rather a family of over 200 distinct conditions that can appear very similar.1 They share the common link of the presence of thick, fibrotic scar tissue that develops over the normal tissues of the lungs. The presence of that fibrotic tissue is what sets PF apart from other interstitial lung diseases, where inflammation or other non-fibrotic thickening of the alveolar membranes causes similar respiratory problems.
As one might expect, given the vast array of processes under the PF umbrella, there is a wide variety of exposures and risk factors associated with the development of a PF condition. According to the Pulmonary Fibrosis Foundation (PFF), these various causes can be grouped into several categories:
- Autoimmune: This form of PF, like other autoimmune conditions, is caused by an over-reaction of the body’s immune system. Antibodies mistakenly attack the tissues of the lungs, causing the inflammation and subsequent scarring that are hallmarks of PF. Certain specific conditions, like rheumatoid arthritis, systemic sclerosis, and Sjögren’s syndrome, are often closely associated with the development of interstitial lung diseases including PF. According to the PF Foundation, autoimmune PF is thought to be one of the most prevalent forms of the condition.
- Environmental/occupational: Another common form of PF is caused by exposure to various atmospheric irritants. This kind of exposure can lead to hypersensitivity pneumonitis, especially when the irritant is an organic antigen (for example, a salmon processing factory with insufficient ventilation led to a cluster of cases of asthma-like symptoms in previously healthy workers due to the aerosolization of fish proteins2). If detected early enough and exposure limited, respiratory symptoms will often fade. Sometimes, though, presentation can be relatively mild and detection delayed. In those cases, fibrotic scar tissue can develop and lead to PF. Airborne fibers, dusts, and other inorganic particles can also lead to fibrosis, leading to case outbreaks not only in animal workers, but people who mine coal, sandblast, or work in other occupations with such contaminants.
- Drug-induced: A variety of medications can also lead to the development of PF. In a cruel twist of fate, this includes some medications that aim to treat the autoimmune issues that also lead to PF, like rheumatoid arthritis. Several other medications, such as amiodarone, biologicals used to treat cancer and immune disorders, and chemotherapy drugs, are also known to potentially cause PF.
- Raditation-induced: Like chemotherapy, radiotherapy used in cancer treatment may lead to pulmonary damage. In these cases, epithelial tissue in the lungs is damaged by the radiation beams, leading to the release of profibrotic mediators, which in turn leads to the development of extracellular matrix proteins (such as collagen) and fibrotic tissue.
- Idiopathic: Unfortunately, in most PF cases, a definite cause can never be established. Idiopathic pulmonary fibrosis is thought to be brought on by a combination of genetic factors, exposure to pollutants, certain concurrent conditions like GERD and pulmonary hypertension, and other risks, but research into why some people with these factors develop IPF and some don’t is still progressing slowly.
Diagnosis of Pulmonary Fibrosis #
As with many chronic respiratory conditions, diagnosis PF can be tricky due to relatively nonspecific symptoms in early stages, which can easily go overlooked. Even when they are noted, they tend to mimic other, more common respiratory conditions. Most people who develop PF do so after turning 50, so age can be a potential exclusion factor. Shortness of breath during activity is, unsurprisingly, one of the key symptoms. A dry, hacking cough may be a warning sign of significant inflammation in the airways, and fast, shallow breathing can suggest the loss of pulmonary compliance due to the buildup of fibrotic tissue, as can certain auscultated lung sounds (specifically crackles/rales). Unintended weight loss can appear as the increased work of breathing and slow deteriorating oxygenation make every breath a fatiguing chore. Poor oxygenation status can also lead to widening and rounding of the fingers and toes, a condition known as digital clubbing. Finally, aching joints and muscles, often a result of inflammation run amok, can be an indicator (in the presence of risk factors and some of the previous symptoms). And, of course, symptoms refractory to front-line therapies for other respiratory problems like COPD or asthmamay also point to PF.
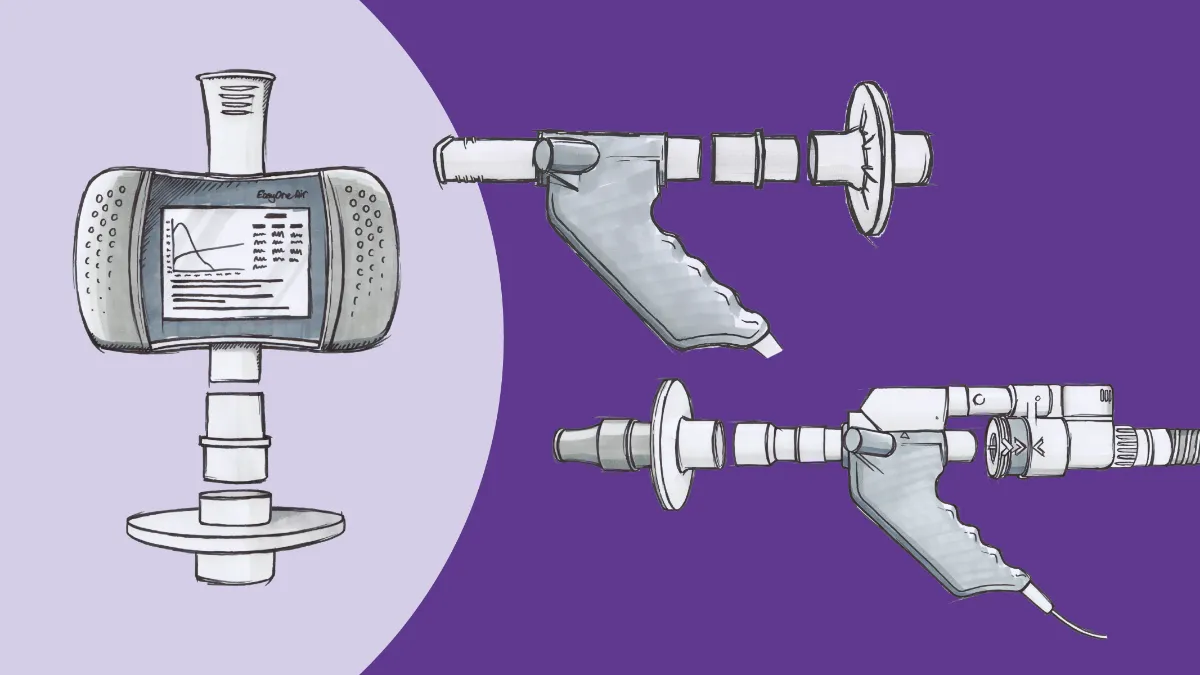
There are several different testing strategies to establish a PF diagnosis. Many people who complain of shortness of breath are first tested by spirometry. This relatively inexpensive, easy-to-perform test can be done in a variety of settings (including primary care) and is therefore easy to implement in practice. A proportional reduction of both the forced expiratory volume in 1 second (FEV1) and the forced vital capacity (FVC) suggests that the test subject is unable to expand their lungs as much as expected.
Spirometry alone is not quite enough to definitively diagnose PF however, as it cannot differentiate between PF and things like thoracic cage abnormalities or insufficient effort. The next step is often a full pulmonary function test, including a test called diffusion capacity of the lung for carbon monoxide, or DLCO. A DLCO test measures how well molecules are able to cross the alveolar membrane by using a tracer gas containing a minute amount of carbon monoxide (owing to CO’s super-affinity for hemoglobin, which facilitates rapid test results). Chest radiography, particularly CT scans, are often the definitive indicator of PF, as fibrotic tissue is readily apparent on these images. Sometimes, the specific type of PF can be determined by careful examination of the patterns seen in these tissues. If a more specific determination is needed, a tissue sample can be removed and biopsied; this can sometimes help determine what pharmacological treatments may be most effective. Other tests, such as pulse oximetry, blood tests, and EKGs can help rule out other causes of shortness of breath, help determine the severity of the disease, or detect deterioration of other organs due to the oxygenation and ventilation issues associated with PF.
What can I do? #
Receiving a diagnosis of pulmonary fibrosis can be tough, but there are an increasing number of treatment options available. New biological compounds help to interrupt inflammatory pathways and otherwise work to decrease the rate of lung function decline. Pulmonary rehabilitation is an excellent (but under-utilized) way to optimize conditioning and maintain both activity tolerance and social interactions. Supplemental oxygen is often used in later stages to help maintain activity levels during and after pulmonary rehab courses. And for the most advanced cases, lung transplantation may be an option.
A variety of support programs and services help keep the PF community thriving as well. The Pulmonary Fibrosis Foundation maintains a network of support groups (currently meeting virtually due to the COVID-19 pandemic), which is searchable on their website at www.pulmonaryfibrosis.org. PFF also has a number of telephone conference groups that meet regularly to discuss specific aspects of living with PF (including one conducted in Spanish), and maintains the PFF Help Center, a clearinghouse of information and resources that is only an email or (toll-free) phone call away.
Of course, September is a perfect time for you to get directly involved! This Pulmonary Fibrosis Awareness Month, you can do things like share 30 PF facts in 30 days on social media, using the hashtags #PFMonth and #BlueUp4PF. You can also wear blue or encourage local business to ‘blue up’ in the official advocacy color for PF, and share those images. This is a prime time for fundraising to support ongoing research and advocacy efforts throughout the entire year, as well.
Whatever method you choose, sharing PF stories as far and wide as possible is one of the most important efforts that can be made to not only put a face on this under-recognized condition, but encourage others to never give up. Happy Pulmonary Fibrosis Awareness Month!
What is Pulmonary Fibrosis | Pulmonary Fibrosis Foundation. https://www.pulmonaryfibrosis.org/understanding-pff/about-pulmonary-fibrosis/what-is-pulmonary-fibrosis. Accessed August 25, 2021. ↩︎
Douglas JD, McSharry C, Blaikie L, Morrow T, Miles S, Franklin D. Occupational asthma caused by automated salmon processing. Lancet. 1995;346(8977):737-740. doi:10.1016/S0140-6736(95)91505-2 ↩︎