The history of PFT - part 3
It’s easy to take pulmonary function testing for granted these days. After all, technology has literally put spirometry in the palm of your hand, and even equipment for more complex testing like diffusion capacity can now be made easily portable. But in order to really understand how remarkable these accomplishments are, it’s important to understand where it all began. This is Part 3 of our ongoing series on the history of pulmonary function testing.
Read from the start:
History of PFT - part 1
History of PFT - part 2
An incentive for treatment #
Lung diseases are nothing new. Descriptions of lungs with what we now call emphysema can be found in some of the earliest known medical textbooks, written up as “voluminous” lungs in Théophile Bonet’s 1679 collection of necropsy reports and medical histories, the Sepulchretum1.1 Tuberculosis as we know it today was identified about the same time, when Richard Morton asserted tubercle-type lesions are always present in the lungs of afflicted patients.2Asthma goes even further back, to where Chinese texts contained descriptions of ‘noisy breathing’ (most likely wheezing) four thousand years ago.3 The search for effective therapies for these conditions has gone on just as long. Not unlike in today’s world, these old-school potential treatments have included the good (compounds of epinephrine analogue ephedrine), the bad (various burning herbal remedies of questionable repute), and the ugly (owl’s blood, honey-soaked millipedes, and various other concoctions).
By the latter half of the 19th century, it was spirometry’s time in the therapeutic limelight. With the link between lung function parameters and overall health generally established, attention turned to practical applications of this evolving technology. Much of the rationale behind using spirometry as a therapeutic option rather than simply diagnostic came from the prevailing idea at the time that respiratory diseases could be separated into diseases of inhalation and those of exhalation Thus, treatment focused on altering the characteristics of the inhaled gas. While oxygen was certainly well-known at this time, and even the potential therapeutic benefits were known, there were few (if any) practical options for delivering supplemental molecular oxygen consistently. The use of “oxygenated bread” and drinking water with oxygen dissolved within were not in the realm of quackery, but referenced in established, respected medical journals as essentially the best option.4Nor were any of the pharmaceutical therapies modern healthcare relies upon available. So, if the composition of inhaled gas couldn’t be changed, that only leaves the pressure and the density.
What comes out, must go in #
That made the spirometer an ideal candidate to deliver therapy. After all, the device was already designed to measure the gas coming out; could it not, with some minor alterations, be used to insufflate a patient with specialized air? Or perhaps change the parameters of their exhalation? This idea came to be known as the Pneumatic Method, and it was the idea behind several new modifications to Hutchinson’s erstwhile device.
One of the first of these devices was known as a pneumatical cabinet. Essentially an airtight iron box, the cabinet also had an inlet where compressed, pressurized air would be pumped in by a steam engine sitting outside. This compressed air had a greater absolute amount of oxygen molecules in it, and the idea that this additional oxygenation would be a boon to various forms of dyspnea.5 Some reports did indeed endorse the use of the cabinet, citing patients seeing relief from things like asthma and bronchitis. Unfortunately, these results were generally short-lived, with patients seeing a return to their baseline not long after leaving their hyperbaric chambers. Considering the remarkable expense of these cabinets, this short-term improvement was simply not worthwhile as anything other than a potential proof-of-concept.
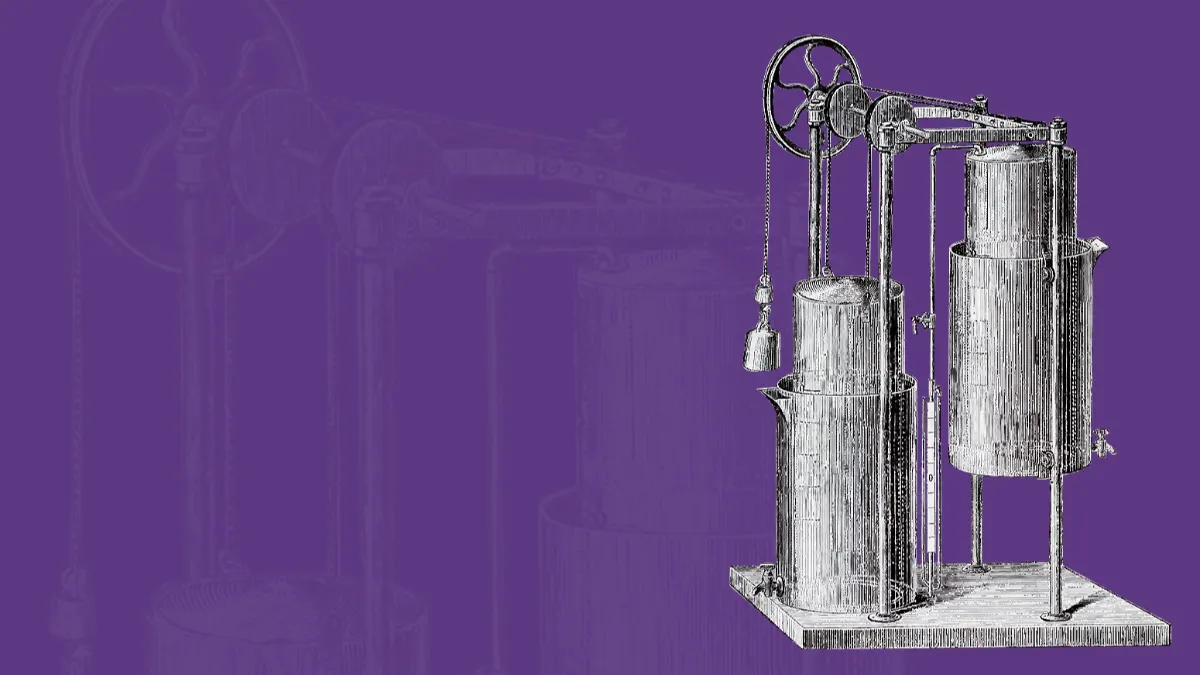
That’s where the spirometer enters the picture. First described by Austrian physician Ignez von Hauke and subsequently improved by Dr. L. Waldenburg of Germany, an apparatus that combined two spirometers modified with weights and pullies could deliver either compressed or rarified air without the use of a dedicated compartment.5 The Hauke Apparatus (and the subsequent Waldenburg enhancements) was still a rather bulky contraption, but was considered portable and inexpensive enough to be far more practical for actual therapy, and was surprisingly similar in concept to aspects of the modern non-invasive ventilator. By adjusting some valves and settings, clinicians could have patients inhaled compressed air and exhale to either ambient pressure or the lower-pressure (and therefore lower resistance) rarified air. This device also offered the ability to introduce inhalation agents such as oxygen or certain fumes thought to be medicinal.
By combining the measurement capabilities of the spirometer with the potential therapeutic benefits of dynamic pressure, clinicians were able to quantify changes in lung parameters, such as vital capacity. This allowed for an evaluation of how therapy might be progressing, as well as greater consistency between encounters, a small initial step toward truly patient-centered care. And, of course, the spirometer values were still available for diagnostic decisions, too. This versatility allowed the Hauke-Waldenburg device to become the dominant spirometer/pneumatic apparatus of the late 19th century, with benefits noted in disease states as varied as tuberculosis, emphysema, and seasonal asthma symptoms.
Building muscle, too #
Additional refinements continued to bring the apparatus to more of the masses, but it was certainly not the only path available to the therapeutic spirometer. The idea of strengthening respiratory muscles, rather than simply forcefully expanding the lungs with pressure, came into vogue. One device in particular, the Lacey Spirometer, positioned itself as a remarkable answer to weak lungs, debility, and various other maladies.6 In the finest tradition of traveling medicine shows, the Lacey claimed to have “no superior” in the treatment of throat problems and obstruction of the bronchial tubes, giving the user a “new and healthy lease on life.” It was a tool that no serious singer or public speaker should do without, lest they be neglectful of “athletic exercise of the lungs.”
In fairness, the Lacey was available with a manometer, allowing for the measurement of expiratory force up to 4 psi. In theory, then, this would make it a predecessor to modern positive expiratory pressure devices. However, the Lacey’s patent doesn’t indicate any actual real resistance, just the ability to measure.7 This put all the effort on the user to blow out at a desired pressure. The lack of standards for normal ranges, what improvements might constitute progress, or really anything else beyond the barest inklings of science to guide its use hampered clinical adoption of the Lacey, exiling it to the back pages of medical periodicals.
Dozens of other devices played with the notions of resistance and measurement to some degree or another. Some, such as multiple devices marketed as the ‘SpiroScope,’ used water and/or sand to measure expiratory force (and potentially offer some degree of expiratory resistance).8 The Deyton Radial Spirometer appeared to use a balance arm to measure both expiratory force and vital capacity, and was marketed again not just toward those with respiratory compromise, but singers and orators.9 Such devices stuck around for quite some time, as it was difficult to argue against their claims that people might benefit in as little as a week…or as long as two years.
The more things change #
The common thread with each of these devices is that they have some foundation in theoretical science, but very little clinical evidence to support their therapeutic benefit. That ties these rudimentary devices more to the modern-day incentive spirometer than the true diagnostic spirometers in use today, but they also represent the first steps toward mainstream recognition of the importance of measuring and working to improve lung function parameters. Lung health was finally on the radar of the general public, rather than just curious scientists and insurance actuaries. Unfortunately, without that clinical backing, spirometers would soon enter something of a dark age with less incentive for spirometer makers to research than to entertain.
Bonet T. Sepulchretum: Sive Anatomia Practica, Ex Cadaveribus Morbo Denatis; Proponens Historias et Observationes Omnium Pene Humani Corporis Affectuum, Ipsorumque Causas Reconditas Revelans; Quo Nomine Tam Pathologiae Genuinae, Quam Nosocomiae Orthodoxae Fundatri. Vol 1.; 1700. https://books.google.com/books?hl=en&lr=&id=PBRBAAAAcAAJ&oi=fnd&pg=PA1&ots=QHDiFdoKXM&sig=a2PMmXJhIQxRqnk3VSHsrS-eQSE. Accessed April 19, 2021. ↩︎ ↩︎
Trail RR. Richard morton (1637—1698). Med Hist. 1970;14(2):166-174. doi:10.1017/S0025727300015350 ↩︎
History of Asthma (Part One): In The Beginning | Asthma.net. https://asthma.net/living/history-of-asthma-part-one-in-the-beginning. Accessed April 22, 2021. ↩︎
Grainge C. Breath of life: The evolution of oxygen therapy. J R Soc Med. 2004;97(10):489-493. doi:10.1258/jrsm.97.10.489 ↩︎
Moore L. The Pneumatic Treatment of Lung Diseases. Med Report. 1892;1:194-195. https://books.google.com/books?id=oxsCAAAAYAAJ&pg=PA194&lpg=PA194&dq=hawke+apparatus+rarified+air&source=bl&ots=J4yYRZbS7m&sig=ACfU3U1kU0yOcdMFp-4rkQGM93d8WOW8PQ&hl=en&sa=X&ved=2ahUKEwjt-Pab-pTwAhXbZc0KHSeWB3AQ6AEwD3oECBwQAw#v=onepage&q=hawke apparatus ra. Accessed April 23, 2021. ↩︎ ↩︎
Official Record: Minutes of the … Session of the Des Moines Annual … - Google Books. https://books.google.com/books?id=QukpAAAAYAAJ&pg=PA165-IA16&lpg=PA165-IA16&dq=lacey%27s+spirometer&source=bl&ots=GWHGAICv_9&sig=ACfU3U30O0K4aPHEkWSuAF9A_-j2NUXK-Q&hl=en&sa=X&ved=2ahUKEwj1p4vO8pfwAhWEXc0KHbxKBMkQ6AEwDnoECAUQAw#v=onepage&q=lacey’s spirometer&f=false. Accessed April 25, 2021. ↩︎
Cranford OF, Sprometer NJ. SPECIFICATION Forming Part of Letters Patent No. Vol 889. ↩︎
Banque d’images et de portraits — BIU Santé, Université de Paris. https://www.biusante.parisdescartes.fr/histoire/images/index.php?mod=s&tout=spirometre. Accessed April 25, 2021. ↩︎
The Esoteric - Google Books. https://books.google.com/books?id=EtUcAQAAIAAJ&pg=PA426&lpg=PA426&dq=deyton+radial+spirometer&source=bl&ots=FHxavv2rYr&sig=ACfU3U3NwfoTeoiPiTF8J_2m-5EgXMdbqg&hl=en&sa=X&ved=2ahUKEwi_14zdspnwAhWBbs0KHaGjAhAQ6AEwDXoECA8QAw#v=onepage&q=deyton radial spirometer&f=false. Accessed April 25, 2021. ↩︎

