Finding the link between lung function and COVID-19
Past studies have shown that people who recover from respiratory viruses may have issues with their lung function and health in the future. Can we expect the same from COVID-19?
As of today, around 15 million people have been diagnosed with the COVID-19 virus, leading to about half a million deaths. Even for people who recover, the impact of the virus has become a real issue. It has caused economic upheaval throughout the globe and has brought terms like “social distancing” to the forefront of everyone’s mind.
While nearly 8 million people have recovered worldwide, that doesn’t necessarily mean individuals who have had the virus are clear of any future conditions or symptoms.
COVID-19 has long been touted as a respiratory issue. Some of the most common symptoms include:
- Coughing
- Sore throat
- Shortness of breath
- Difficulty breathing
Needless to say, the context of lung health and recovery after the virus is of the utmost importance.
How has lung function been studied for past illnesses? #
Unfortunately, there is limited data on the potential long-term effects of a respiratory illness on lung function. One such instance we can look at is the SARS outbreak that impacted many areas around the world in 2003.
A study performed with 110 SARS survivors at the Prince of Wales Hospital was performed to examine the illness’ impact on lung function, exercise capacity, and health-related quality of life.
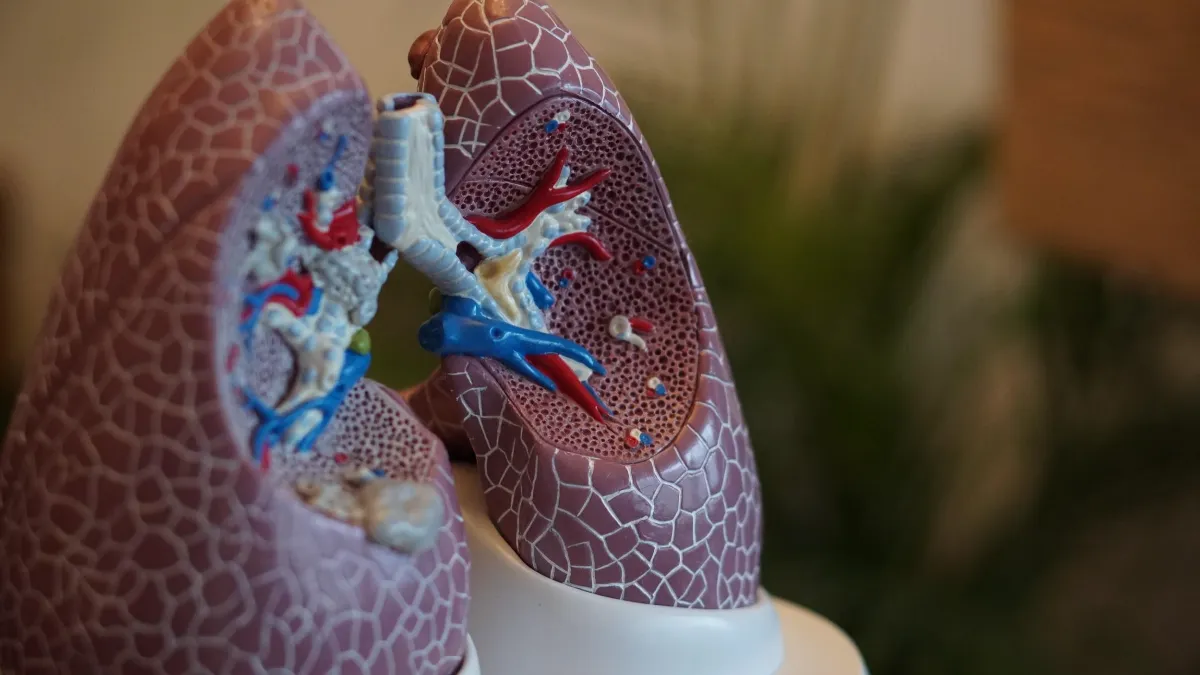
What this study discovered was that both the exercise capacity and health-related quality of life was lower than the normal population six months after recovering from the disease. Using spirometry, it was also discovered that these survivors had significantly decreased lung function. DLCO was heavily-impacted, followed by TLC.
Lung function in COVID-19 survivors #
It may still be too early to tell what the long-term impact of COVID-19 will be on the lungs, especially in those who may have already had underlying conditions or compromised immune systems. However, we are beginning to get some early indicators as to how this virus impacts lung health after someone recovers.
One study of 18 COVID-19 survivors discovered that five non-severe patients and two severe patients had abnormal lung function. Of the 12 non-severe cases that were tested, five of them had small airway dysfunction, while three had obstructive ventilation impairment.
This study was performed using spirometry on all patients to test their lung function. The dysfunction of the airways in these patients is a clear indicator that more research needs to be done on the long-term effects of COVID-19 and the lungs.
If we can learn anything from past viruses and how they impacted lung function, we should be conscious that even patients who survive the Coronavirus may have years of poor lung capacity to deal with. This study shows that there is an impairment of diffusion capacity. As such, lung function tests like DLCO and spirometry should be standard procedure for those who have recovered from COVID-19.
An additional risk is the development of Acute Respiratory Distress Syndrome (ARDS) in COVID-19 survivors. This is a syndrome in which the air sacs in the lungs fill up with fluid, severely limiting diffusion capacity. Early diagnosis of COVID-19 is one of the best ways to monitor the potential symptoms of ARDS and how the two might be related, but it is still too soon to tell if there will be any long-term effects that link the two.
What does this mean for survivors? #
Again, while more testing needs to be done to determine how COVID-19 impacts the lung function of survivors, one thing is sure; DLCO and spirometry should be part of routine examinations for COVID-19 survivors, not only shortly after the disease itself has passed, but for years to come. In some cases, lung capacity and diffusion may not be affected for years. We are still learning about the long-term impact of viruses and outbreaks that happened almost 20 years ago, thanks to consistent studies that have been performed over the years.
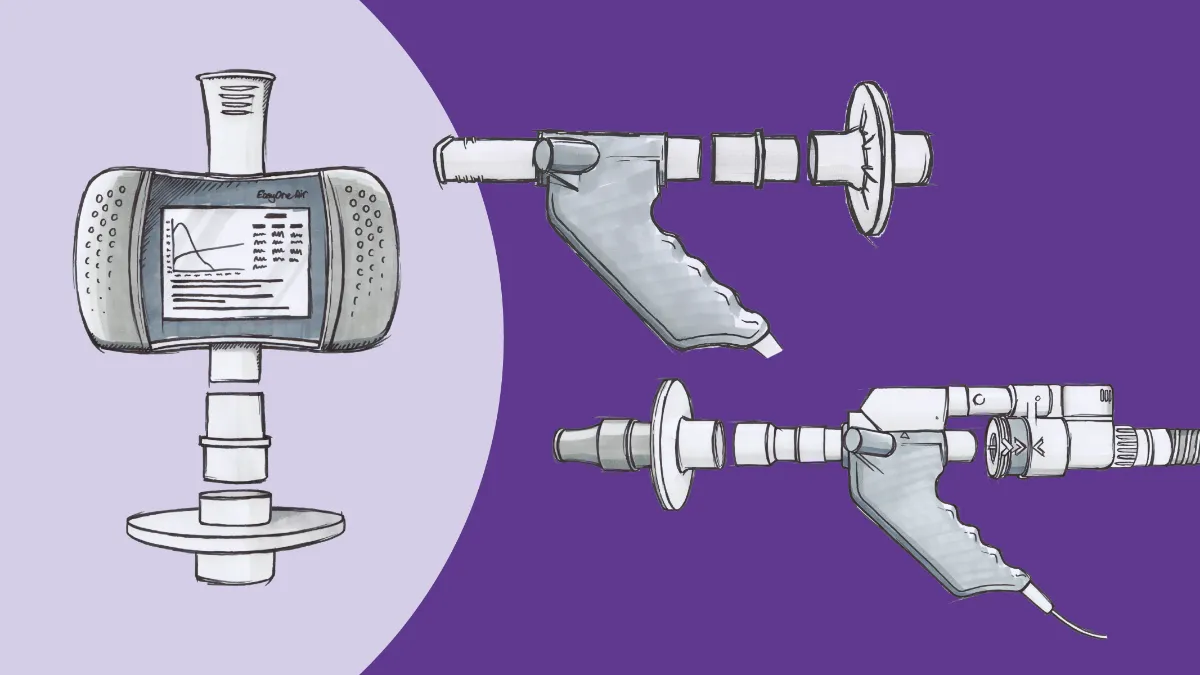
These types of tests can serve as monitoring tools for survivors, and provide doctors with the necessary information to prepare patients with lung conditions. The more testing that is done on survivors, the sooner lung disease can be discovered, and those survivors can begin treatment. Of course, the easiest ways to monitor patients are with lung function tests that should be performed at the point of care, rather than asking those who have already been through COVID-19 to go to a hospital for testing.
For more than 20 years ndd has worked to improve the early detection and accurate diagnosis for people living with COPD and other chronic lung diseases with the EasyOne products—by supporting research, helping to create awareness, launching innovative products, and making them available to over 100 countries.
The EasyOne product line was developed for physicians to offer accurate and reliable diagnosis at the point of care and start immediate treatment. This helps avoid irreversible lung damage for millions of patients while significantly reducing healthcare costs.
To learn more visit: EasyOne Product Solutions