Asthma-COPD Overlap

A question of certainty #
Medicine loves certainty. Certainty gives us the ability to make a diagnosis, to put an absolute, discrete label on a set of symptoms, and to develop a treatment plan to ameliorate those symptoms. Being certain about a diagnosis allows us to set goals for research and development, and it provides for the monitoring of progress along the way. In short, being confident in a diagnosis allows clinicians to have a ‘right answer’ to their patients’ questions, which is a very comfortable place to be.
The human body is funny, though. It is a solidly analog machine in an increasingly digital world. When things go awry, they rarely do so in a binary, on/off sort of way. Instead, there are ranges of pathological processes influencing and interacting with one another. Manifestations of all these processes can appear, suddenly making a diagnosis not just right or wrong, but a little bit of both. Such is the case with the overlap between asthma and COPD.
The clinical dilemmas #
Ironically, much of the ambiguity involved with asthma-COPD overlap (ACO) comes from the search for clarity itself. Definitions are continually revisited and revised, making it difficult to determine how many people are impacted. A 2019 meta-analysis that included 27 peer-reviewed, population-based studies found that roughly 2% of the global population, a total of 158 million people, may be affected.1 However, the study also describes how the variety of diagnostic criteria used in those studies made it very difficult to have certainty in that prevalence. Even closely-related international groups such as the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) disagree on criteria, with GINA advocating for a stepwise diagnostic approach that considers whether patients have features of either (or both) condition(s),2 and GOLD barely mentioning overlap at all.3 With no globally-accepted description in place, clinicians are often left on their own to evaluate and treat patients presenting with dyspnea, cough, and allergy symptoms, leaving some patients to be potentially undertreated for years.
Even in cases where an appropriate diagnosis is made, a similar ambiguity exists in the treatment of asthma-COPD overlap. Inconsistent descriptions of the process have limited our ability to research the condition, and it has been similarly difficult to develop laboratory models of the mechanisms to create the intertwined clinical features.4 That makes it difficult to determine whether the overlap population is most effectively treated by asthma strategies, COPD strategies, or a combination of both. Considering the overlap between these therapeutic worlds, there is also often concern that ACO may simply be a distinction without a practical difference.
However, the difference may be more important than we yet realize. Utilization review studies are already pointing to significantly increased use of emergency-department visits and hospital admissions by those people with features of ACO compared with not only the general public, but those diagnosed with either condition individually.5 Other studies have demonstrated that those in the ACO population tend to have lower health quality indicators of nearly every type, from increased medication usage to lower healthcare-related quality of life measures to higher symptom burden.6 Clearly, identifying ACO earlier and developing individualized treatment strategies will be essential to improving the health of those who live with it.
ndd PFT solutions #
That’s where PFT solutions from ndd come in. Even in conditions where the formal definition is clouded (like ACO), patients will have recognizable, treatable traits that allow you to select therapies that can optimize their quality of life and minimize their risk for exacerbations.
Easy to use pulmonary function devices #
With the ndd EasyOne line of pulmonary function testing equipment, you have immediate access to key tests like spirometry (essential for detecting airflow obstruction and determining whether it is reversible) and diffusion capacity (allowing differentiation between asthma, COPD, and other respiratory conditions, as well as their severity), no matter what your practice setting.
Focus on your patient #
ndd’s cutting-edge TrueCheck and TrueFlow technologies allow you to be confident in test results without time-consuming calibration checks and with minimal annual maintenance requirements. With EasyOne devices, you no longer have to spend time worrying about your devices or your data. Instead, you and your staff can spend your time doing what you do best: Caring for your patients.
The future of asthma-COPD overlap #
The future will bring more clarity to the world of asthma-COPD overlap. As the condition becomes better understood, clinicians will have more tools at their disposal to get the elusive ‘right answer’ for their patients. Chest imaging, bronchoprovocation studies, exhaled nitric oxide analyses, and other specialized testing techniques are continuing to shed light on the mysteries of the overlap, perhaps even permanently defining it as a discrete syndrome. As the pathophysiologies under the surface of ACO become clearer, optimal therapy regimens will become more well-defined as well, once again providing certainty in clinical decision making. Until then, you can count on ndd solutions to help you provide the best possible care.


EasyOne Air
Portable & PC spirometer
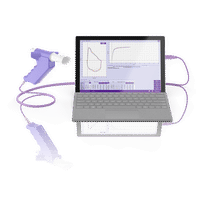

Easy on-PC
PC spirometer
Hosseini M, Almasi-Hashiani A, Sepidarkish M, Maroufizadeh S. Global prevalence of asthma-COPD overlap (ACO) in the general population: A systematic review and meta-analysis. Respir Res. 2019;20(1):1-10. doi:10.1186/s12931-019-1198-4 ↩︎
GLOBAL STRATEGY FOR ASTHMA MANAGEMENT AND PREVENTION Updated 2020.; 2020. Accessed October 15, 2020. www.ginasthma.org ↩︎
Global strategy for diagnosis management and prevention of C. 2021 GOLD Reports - Global Initiative for Chronic Obstructive Lung Disease - GOLD. Published 2021. Accessed May 13, 2021. https://goldcopd.org/2021-gold-reports/ ↩︎
Tu X, Donovan C, Kim RY, Wark PAB, Horvat JC, Hansbro PM. Asthma-COPD overlap: Current understanding and the utility of experimental models. Eur Respir Rev. 2021;30(159). doi:10.1183/16000617.0185-2019 ↩︎
Kim M, Tillis W, Patel P, Davis RM, Asche C V. Association between asthma/chronic obstructive pulmonary disease overlap syndrome and healthcare utilization among the US adult population. Curr Med Res Opin. 2019;35(7):1191-1196. doi:10.1080/03007995.2019.1565531 ↩︎
Wurst KE, St. Laurent S, Hinds D, Davis KJ. Disease Burden of Patients with Asthma/COPD Overlap in a US Claims Database: Impact of ICD-9 Coding-based Definitions. COPD J Chronic Obstr Pulm Dis. 2017;14(2):200-209. doi:10.1080/15412555.2016.1257598 ↩︎