Relevance of DLCO and lung function testing for optimized patient management in Long COVID
Abstract/Executive Summary #
The SARS-CoV-2 virus represents a global health crisis. The acute disease caused by the virus, COVID-19, has had a massive impact on healthcare systems worldwide, with increased hospitalizations and intensive care unit bed utilization. However, these acute care impacts represent only the beginning of COVID-19’s overall footprint. There is now a growing population of COVID-19 survivors with prolonged post-acute symptoms, a syndrome often described as “Long COVID.” These symptoms are predominantly related to respiratory impairments, but also include neurological issues, cardiovascular complications, and chronic fatigue.
Research has suggested a link between COVID-19 and diffusion capacity of the lung for carbon monoxide (DLCO). These changes are thought to be caused by a combination of changes in the lung parenchyma combined with a variety of pathophysiologies in the pulmonary vasculature. Importantly, these changes can appear without a concomitant degree of airflow restriction on spirometry and are also present in a significant number of non-hospitalized COVID-19 patients. Best available data suggest over one-third of patients with these so-called mild cases fail to return to their baseline health status weeks after the onset of their symptoms.
Clinical rehabilitation programs to support COVID-19 survivors (whether hospitalized or not) are being established in many countries, with some already accepting patients. Patients utilizing these programs have demonstrated improved DLCO as well as other lung function and quality of life assessments. Considering that many patients with mild cases may not realize they have been infected until their symptoms fail to resolve, DLCO measurements are an essential tool for diagnosing COVID-19-related respiratory impairments. DLCO may also be used as a quality improvement tool for rehabilitation programs. Utilization of DLCO testing should be scaled up as rapidly as possible to improve outcomes and provide more efficient care across the healthcare continuum.
Background #
General Situation
The current pandemic of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) represents a global health crisis. Infection with SARS-CoV-2 in humans is associated with a broad spectrum of clinical respiratory syndromes.1 This has caused a sudden increase in hospitalizations across the globe. The clinical manifestations vary based upon the severity of the disease in individuals. approximately 80% of patients experience mild manifestations, 15% experience severe manifestations, and 5% endure critical cases. Consequently, the COVID-19 pandemic has increased the demand for post-acute care in patients across the continuum of disease severity.2
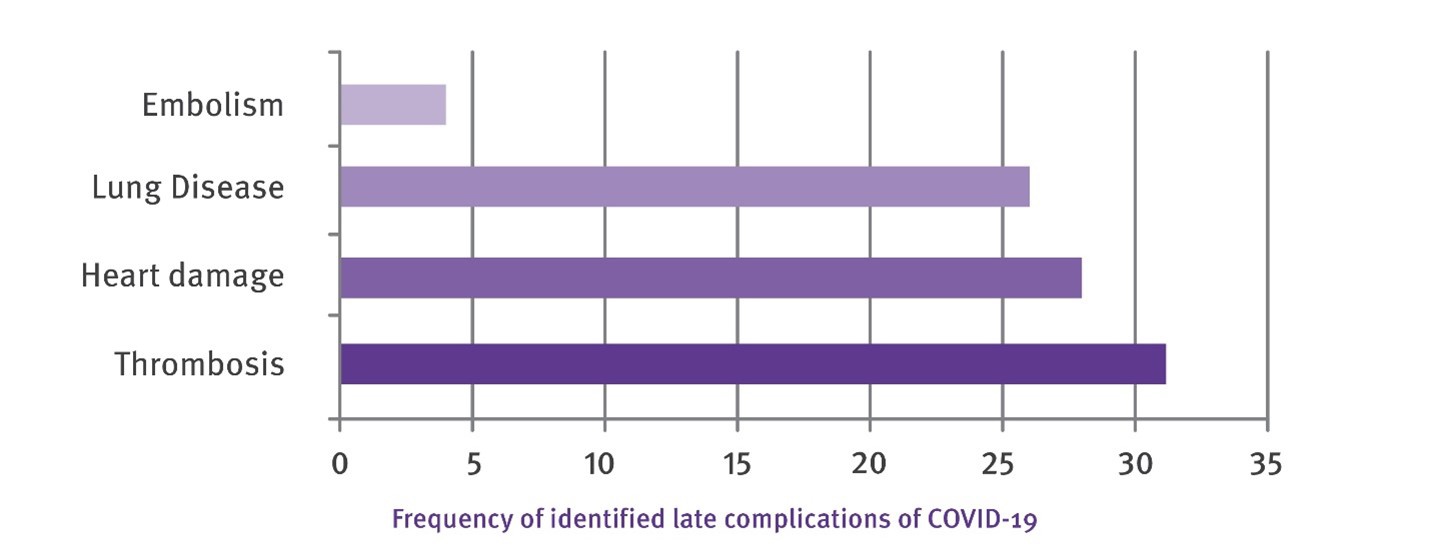
The high number of COVID-19 cases worldwide has resulted in a large population of survivors with prolonged post infection symptoms. The table below shows the frequency of the most common late complications. Notably, lung disease is the most common long-term complication reported.3
Clinical programs designed to care for individuals previously hospitalized with COVID-19 are being developed, with some in initial phases of operation. These post-COVID programs include patients who required critical care support during their inpatient stay as well as non-hospitalized individuals with persistent respiratory symptoms.4 Similar programs are established or prepared worldwide.5
Link between COVID & DLCO #
Imaging and morphology of COVID-19 lungs
The lungs from patients with COVID-19 show distinctive pathophysiological markers in the vasculature, consisting of severe endothelial injury associated with the presence of intracellular virus as well as damaged cell membranes. Histologic analysis of pulmonary vessels in patients with COVID-19 showed widespread thrombosis with microangiopathy.6 Lins et al7 used automated quantitative CT scans to measure small blood vessel volume and pulmonary vascular density. The authors found striking anomalies in the distribution of blood volume within the pulmonary vascular tree in COVID-19 patients, consistent with increased pulmonary vascular resistance in vessels below the resolution of CT.
(See figure 3)
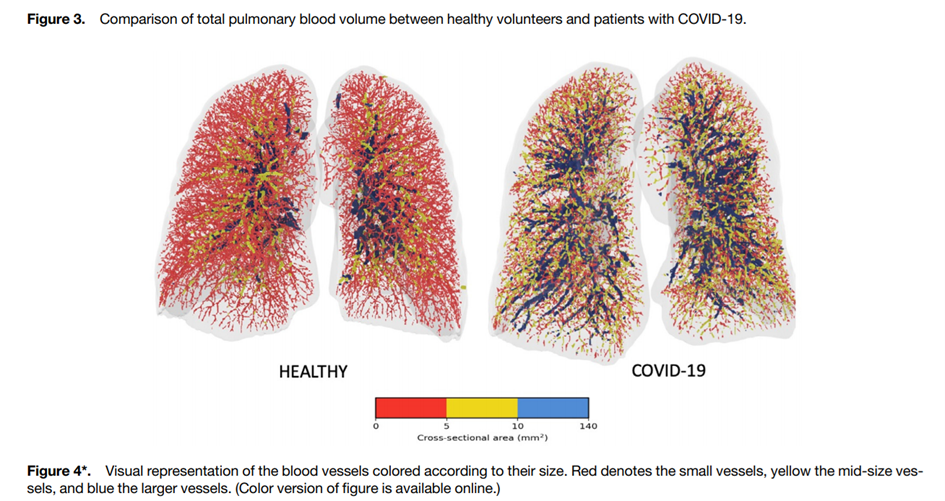
*Muriel Lins, MD, Jan Vandevenne, MD, Muhunthan Thillai et al. Assessment of Small Pulmonary Blood Vessels in COVID-19 Patients Using HRCT. Academic Radiology, Vol 27, No 10, October 2020
In COVID-19 cases, diffuse endothelial inflammation, dysfunction, and apoptosis resulting from a direct viral infection of the endothelial cells have been seen within the lungs and other organs. Provencher et al8 suggest that COVID-19 impacts the pulmonary circulation and survivors of severe COVID-19 may experience persistent impairment in pulmonary gas exchange. These patients often demonstrate mild restrictive patterns on pulmonary function tests and their impaired diffusion capacity may also partly be of vascular origin.8
The severity of the disease is reflected by DLCO measurements during post-COVID
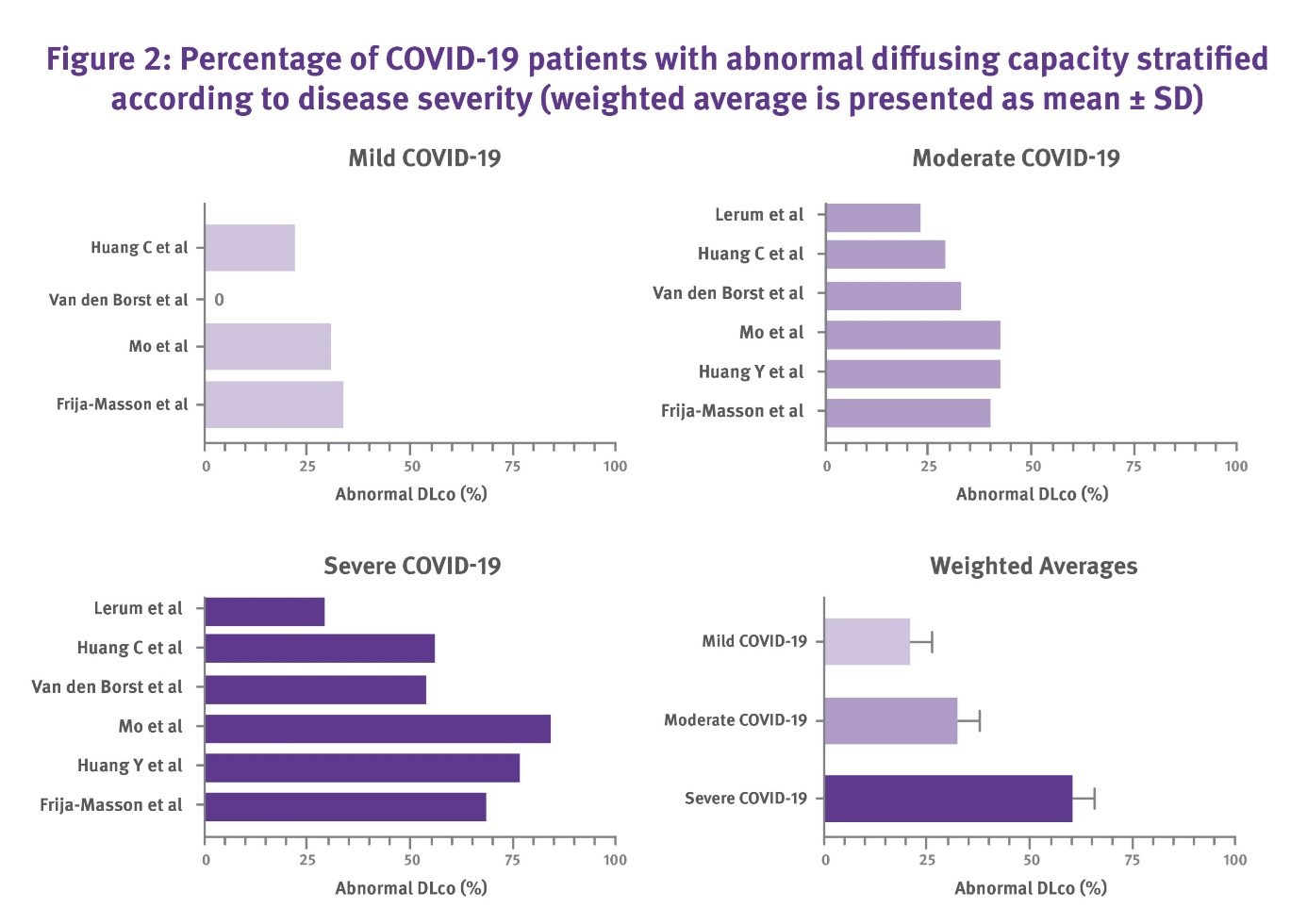
Within a short period (less than one year during the pandemic), a significant number of papers were published about pulmonary function in patients with COVID-19 after discharge from the hospital (see Annex 1). In all publications, the authors consistently observed a more pronounced impairment of DLCO compared to appearances of restrictive spirometry patterns, supporting the relevance of DLCO measurements in COVID-19 management. The figure below presents an overview of the significant number of patients with abnormal DLCO after experiencing mild, moderate and severe cases of Covid-19 respectively.9
Importance and applications of pulmonary function testing including DLCO after the acute phase #
Rehabilitation of hospitalized COVID-19 patients
Impairment of DLCO reflects the pulmonary sequelae of COVID-19. Fortunately, rehabilitation programs have been demonstrated to improve DLCO and initial published reports have shown that rehabilitation programs improve outcome on long COVID patients.10 It is now well established that DLCO is a sensitive indicator to assess the severity of the infection.
Liu et al11 conducted a randomized controlled study on the impact of pulmonary rehabilitation in 36 male and female patients recovering from COVID-19 (age: 69 ± 8 years). DLCO and 6MWT distance improved by approximately 30% vs controls with 6 weeks of respiratory muscle training.
Puchner et al12 found that multidisciplinary rehabilitation resulted in a significant improvement in lung function, as reflected by an increase of forced vital capacity (FVC) (p=0.007), forced expiratory volume in one second (FEV1)(p=0.014), total lung capacity (TLC) (p=0.003), and diffusion capacity for carbon monoxide (DLCO) (p=0.002). They concluded that individuals discharged after a severe case of COVID-19 frequently present with persistent physical and cognitive dysfunction after hospital discharge. Those patients significantly benefit from multi-disciplinary inpatient rehabilitation programs. DLCO measurements could therefore have a major positive impact on patient outcomes by ensuring that long term effects are detected rapidly, allowing rehabilitation to start as early as possible. This is especially important for patients that were never hospitalized but might still suffer from long term effects. Additionally, serial DLCO measurements could potentially be used to improve and refine rehabilitation programs over time, as ongoing measurements and trends provide insight into the effectiveness of different methods used in various rehabilitation strategies.
Long COVID in patients that have not been hospitalized
The majority of patients with COVID -19 have relatively mild disease manifestations and consequently are generally not hospitalized. Many may not fully realize they even experienced COVID-19 until they fail to see symptom improvement. As of today, only sparse data are available about the long-term course of the disease in these cases. According to a survey done by the Centers for Disease Control and Prevention (CDC), 35% of non-hospitalized patients with mild COVID-19 cases failed to return to baseline health 14 to 21 days after their symptoms started.12
The large number of patients suffering from Long COVID that have never been hospitalized13, in combination with the significant change seen in DLCO even in mild COVID-19 cases9 strongly suggests that DLCO should be performed as a routine measurement on all COVID-19 patients with prolonged symptoms, as an additional objective measure to assess potential lung damage and to assess the potential need for a rehabilitation program.
ANNEX 1 – Publications showing the relation between DLCO and severity of COVID-19 #
Torres- Castro et al14 recently summarized published respiratory function in 380 patients post infection by COVID-19. In the sensitivity analysis, they found a prevalence of 0.39 for impaired DLCO, 0.15 for a restrictive pattern, and 0.07 for altered obstructive pattern.
Sonnweber T et al15 published an observational prospective multi-centre trial on cardiopulmonary recovery in 145 COVID-19 patients, 60 and 100 days after confirmed diagnosis. 41% of all subjects exhibited persistent symptoms 100 days after COVID-19 onset, with dyspnoea being most frequent (36%). Patients had impaired lung function, with a reduced diffusing capacity being the most prominent finding (21% of subjects).
Van der Sar et al16 performed a prospective cohort study in 101 patients six weeks post-discharge. Subjects underwent interviews and pulmonary function tests. Diffusion limitation (DLCO < 80% of predicted value) was found in 66 (71.7%) of 92 cases, obstruction in 26 (25.7%) of 101, and restriction in 21 (21.2%) of 99. Diffusion capacity was significantly lower in cases after severe pneumonia. FEV1 and DLco showed significant positive correlations with mMRC scores and multiple SF-36 domains, especially physical functioning.
Guler et al17 performed the Swiss COVID-19 lung study, a multicentre prospective cohort of 113 COVID-19 survivors were included (mild/moderate 47, severe/critical 66) investigating pulmonary sequela of COVID-19. After four months, impairments in pulmonary function and physical performance were more pronounced in patients with previously severe and critical COVID-19 courses, compared to those with mild and moderate illness. Specifically, DLco %-predicted at four months was the most important, independent correlate of a more severe initial disease.
Zhao et al18.18 reveal that radiological and physiological abnormalities were prevalent in a considerable proportion of COVID-19 survivors that did not require intensive care 3 months after discharge. A higher level of D-dimer on admission could effectively predict impaired DLco after 3 months from discharge.
Shah et al.19 conducted a study on 60 COVID patients 12 weeks after the onset of their symptoms and demonstrated the clinical, radiological, and pulmonary function abnormalities. Thereafter they identified clinical predictors of respiratory outcomes. At least one pulmonary function variable was abnormal in 58% of patients and 88% had abnormal imaging on chest CT. A strong association was observed between days on oxygen supplementation during the acute phase of COVID-19 and both DLCO12 and total CT score.
This paper is supported by Prof. Dr. Helgo Magnussen member of the advisory board of ndd.
Huertas A, Montani D, Savale L, et al. Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)? Eur Respir J. 2020;56(1). ↩︎
Klok FA, Boon G, Barco S, et al. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020;56(1). ↩︎
SeyedAhmad SeyedAlinaghi, AmirMasoud Afsahi2,MehrzadMohsseniPour et al. Late Complications of COVID-19; a Systematic Review of Current Evidence. Archives of Academic EmergencyMedicine. 2021; 9(1) ↩︎
Lutchmansingh DD, Knauert MP, Antin-Ozerkis DE, et al. A Clinic Blueprint for Post-Coronavirus Disease 2019 RECOVERY: Learning From the Past, Looking to the Future. Chest. 2021;159(3):949-958. ↩︎
Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19: Interim Guidance on Rehabilitation in the Hospital and Post-Hospital Phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force. Eur Respir J. 2020. Barker-Davies RM, O’Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949-959. ↩︎
Maximilian Ackermann, Stijn E Verleden, Mark Kuehnel et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med 2020 Jul 9;383(2) ↩︎
Muriel Lins, MD, Jan Vandevenne, MD, Muhunthan Thillai et al. Assessment of Small Pulmonary Blood Vessels in COVID-19 Patients Using HRCT. Academic Radiology, Vol 27, No 10, October 2020 ↩︎
Steeve Provencher, Francois Potus and Sébastien Bonnet et al. COVID-19 and the pulmonary vasculature. Pulmonary Circulation 2020 ↩︎ ↩︎
Max Thomas, Oliver J. Price, James H. Hull. Pulmonary function and COVID-19. Current opinion in physiology March 2021. ↩︎ ↩︎
Kai Liu, Weitong Zhang, Yadong Yang, et al. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complementary Therapies in Clinical Practice Volume 39, May 2020. Bernhard Puchner, Sabina Sahanic, Rudolf Kirchmair, Alex Pizzini. Beneficial effects of multi-disciplinary rehabilitation in post-acute COVID-19 - an observational cohort study. January 2021European Journal of Physical and Rehabilitation Medicine. ↩︎
Kai Liu, Weitong Zhang, Yadong Yang, et al. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complementary Therapies in Clinical Practice Volume 39, May 2020. ↩︎
Bernhard Puchner, Sabina Sahanic, Rudolf Kirchmair, Alex Pizzini. Beneficial effects of multi-disciplinary rehabilitation in post-acute COVID-19 - an observational cohort study. January 2021European Journal of Physical and Rehabilitation Medicine. ↩︎ ↩︎ ↩︎
Mark W. Tenforde, Sara S. Kim, Christopher J. Lindsell et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network. Centers for disease control and prevention, Morbidity and Mortality Weekly Report (MMWR) July 31, 2020 / 69(30). ↩︎
Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, et al. Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis. Pulmonology. 2020. ↩︎
Sonnweber T, Sahanic S, Pizzini A, et al. Cardiopulmonary recovery after COVID-19 - an observational prospective multi-center trial. Eur Respir J. 2020. ↩︎
van der Sar-van der Brugge S, Talman S, Boonman-de Winter L, et al. Pulmonary function and health-related quality of life after COVID-19 pneumonia. Respir Med. 2021;176:106272. ↩︎
Guler SA, Ebner L, Beigelman C, et al. Pulmonary function and radiological features four months after COVID-19: first results from the national prospective observational Swiss COVID-19 lung study. Eur Respir J. 2021. ↩︎
Zhao YM, Shang YM, Song WB, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;25:100463. ↩︎ ↩︎
Shah AS, Wong AW, Hague CJ, et al. A prospective study of 12-week respiratory outcomes in COVID-19-related hospitalisations. Thorax. 2020. ↩︎






